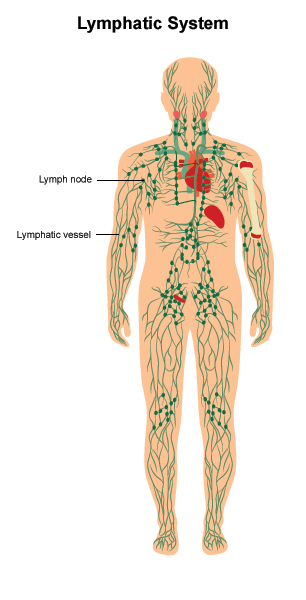
Lymphedema is the abnormal buildup of fluid in soft tissue. It is caused by a blockage in the body's lymphatic system. The lymphatic system helps fight infection and other diseases is made up of:
Lymph or lymphatic fluid. A colorless fluid containing white blood cells.
Vessels. A network of thin tubes that carry lymph throughout the body.
Lymph nodes. Small, bean-shaped glands that filter bacteria and other harmful substances out of the lymphatic fluid. Lymph nodes are found throughout the body.
When lymph nodes are removed or damaged, lymphatic fluid can collect in the surrounding tissue and make them swell.
Lymphedema may develop immediately after surgery or radiation therapy. Or, it may occur months or even years after cancer treatment has ended. Most often, lymphedema affects an arm or leg. But it can also happen in the neck, face, mouth, abdomen, groin, or other parts of the body.
Treating and relieving side effects is an important part of cancer care and treatment. This is called palliative and supportive care. Talk with your health care team about any symptoms you have, including new symptoms or changes.
What are the symptoms of lymphedema?
The symptoms of lymphedema depend on the part of the body that is affected. Lymphedema in an arm or leg may cause the following symptoms:
-
Swelling or a heavy feeling
-
Weakness or less flexibility
-
Rings, watches, or clothes that become too tight
-
Discomfort or pain
-
Tight, shiny, warm, or red skin
-
Hardened skin that does not indent when pressed or thicker skin
-
Skin that looks like an orange peel (swollen with small indentations)
-
Small blisters that leak clear fluid
Lymphedema in the head and neck may cause the following symptoms:
-
Swelling of the eyes, face, lips, neck, or area below the chin
-
Discomfort or tightness
-
Difficulty moving the neck, jaw, or shoulders
-
Thickening and scarring of the skin on the neck and face, called fibrosis
-
Decreased vision because of swollen eyelids
-
Difficulty swallowing, speaking, or breathing
-
Drooling or dropping food from the mouth while eating
-
Nasal congestion or long-lasting middle ear pain, if swelling is severe
Symptoms of lymphedema may begin slowly and are not always easy to detect. Sometimes the only symptoms may be heaviness or aching in an arm or leg. Other times, lymphedema may begin more suddenly.
What are the causes of lymphedema?
Lymphedema can occur in people with many types of cancer, including bladder, breast, head and neck, ovarian, penile, and prostate cancers. Lymphedema can be a long-term side effect of some cancer treatments. The most common causes of lymphedema in cancer survivors include:
-
Surgery in which lymph nodes were removed. For example, surgery for breast cancer often involves removing 1 or more lymph nodes under the arm to check for cancer. Lymph node removal can cause lymphedema in the arm.
-
Radiation therapy or other causes of inflammation or scarring in the lymph nodes and lymph vessels
-
Blockage of the lymph nodes and/or lymph vessels by the cancer
The risk of lymphedema increases with the number of lymph nodes and lymph vessels removed or damaged during cancer treatment or biopsies. Sometimes lymphedema is not related to cancer or its treatment. For instance, a bacterial or fungal infection or another disease involving the lymphatic system may cause this problem.
How is lymphedema diagnosed?
A doctor is often able to find lymphedema by looking at the affected area. But sometimes they will recommend additional tests to confirm a diagnosis, plan treatment, or rule out other causes of the symptoms. These tests may include:
Measurements. Measurements will be taken of the affected body part to monitor the swelling. The affected arm or leg can also be placed into a tank of water to calculate the volume of fluid that has built up.
Lymphoscintigraphy. This is an imaging method that creates a picture of the lymphatic system. This is a reliable test, but it is not commonly used.
Ultrasound. The flow of fluid through the lymph system can be seen using an ultrasound. This imaging test uses sound waves to create a picture of the inside of the body. An ultrasound can also be used to rule out blood clots as a cause of the swelling.
Computed tomography (CT or CAT) scan or magnetic resonance imaging (MRI). A CT scan or an MRI can be used to show the pattern of lymph drainage. They will show if a tumor or other mass is blocking the flow of the lymphatic system. Doctors do not usually use CT or MRI scans to diagnose lymphedema unless they are concerned about a possible cancer recurrence.
Other tools. Other tools used to diagnose lymphedema include perometry, which uses infrared light beams, or a bioimpedance spectroscopy, which measures electrical currents flowing through body tissues.
It is also important to make sure another illness is not causing the swelling. Your doctor may perform other tests to rule out heart disease, blood clots, infection, liver or kidney failure, or an allergic reaction.
What are the stages of lymphedema?
Lymphedema is described using stages, from stage 0 to stage III (3). Stage 0 is considered mild lymphedema and stage III is considered severe.
Stage 0. Swelling usually cannot be seen, even though the lymphatic system has already been damaged. Some people may feel heaviness or aching in the affected body part. This stage may last months or even years before swelling occurs.
Stage I. Swelling is visible but can be reduced by keeping the affected limb and using compression (see "How is lymphedema managed and treated?" below). The skin may indent when pressed. There are no visible signs of skin thickening and scarring.
Stage II. The skin may or may not indent when it is pressed, but there is moderate to severe skin thickening. Compression and keeping the affected limb raised may help a little but will not reduce swelling.
Stage III. The skin has become very thick and hardened. The affected body part has swollen in size and volume. The skin has changed texture. Stage III lymphedema is permanent.
How is lymphedema managed and treated?
Although treatment can help control lymphedema, it currently does not have a cure. Lymphedema treatments can:
-
Reduce swelling
-
Prevent lymphedema from getting worse
-
Prevent infection
-
Improve your ability to function
-
Improve how the affected body part looks
Your doctor may recommend a certified lymphedema therapist (CLT). The CLT can develop a treatment plan for you, which may include:
Manual lymphatic drainage (MLD). MLD involves gentle skin massage. It helps blocked lymphatic fluid drain properly into the bloodstream and may reduce swelling. For best results, you should begin MLD as close to the start of lymphedema symptoms as possible. A member of your health care team can refer you to a CLT trained in this technique.
Exercise. Exercising usually improves the flow of lymph fluid through the lymphatic system and strengthens muscles. A CLT can show you exercises to improve your range of motion. Ask your doctor or therapist when you can start exercising and which exercises are right for you.
Compression. Non-elastic bandages and compression garments, such as elastic sleeves, place gentle pressure on the affected area. This helps prevent fluid from refilling and swelling after decongestive therapy (see below). Compression garments must fit properly and should be replaced every 3 to 6 months.
Skin care. Lymphedema can increase the risk of infection. Keep the affected area clean, moisturized, and healthy. Apply moisturizer each day to prevent chapped skin. Avoid cuts, burns, needle sticks, or other injury to the affected area. If you shave, use an electric razor to reduce the chance of cutting the skin. When you are outside, wear a broad-spectrum sunscreen that protects against both UVA and UVB radiation and has a sun protection factor (SPF) of at least 30. If you do cut or burn yourself, wash the injured area with soap and water and use an antibiotic cream as directed by your health care team.
Complete decongestive therapy (CDT). This is also known as complex decongestive therapy. CDT combines skin care, manual lymphatic drainage, exercise, and compression. A doctor who specializes in lymphedema or a CLT should do this therapy. The therapist will also tell you how to do the necessary techniques by yourself at home and how often to do them. Ask your doctor for a referral.
Elevation. Keeping your affected limb raised helps to reduce swelling and encourage fluid drainage through the lymphatic system. But it is often difficult to keep a limb raised for a long time.
Lower-level laser treatments (LLLT). A small number of clinical trials have found that LLLT could provide some relief from lymphedema after removal of the breast, particularly in the arms.
Medications. Your doctor may prescribe antibiotics to treat an infection or a medication to relieve pain.
Physical therapy. If you have trouble swallowing or other issues from lymphedema of the head and neck, physical therapy may be able to help.
How to reduce your risk of lymphedema
Talk with your doctor if you have concerns about developing lymphedema. Also, try the following tips:
Maintain a healthy weight. Take positive steps to maintain your weight after a cancer diagnosis. This may help lower your risk of developing lymphedema.
Change your position. Avoid sitting or standing for a long time. While sitting, avoid crossing your legs. It may also help to lift yourself up with pillows in bed. An upright position improves lymph drainage.
Wear loose-fitting clothes. Tight-fitting clothing can cause fluid to build up. If you are at risk of developing head and neck lymphedema, do not wear tops with a tight neckline. For those at risk for developing leg lymphedema, protect your feet by wearing closed-toed shoes. Avoid flip-flops and sandals. For those at risk of arm lymphedema, avoid wearing tight clothing and jewelry that pinches or squeezes your arm or hand, like a tight sleeve or bracelet.
Limit time in extreme heat or cold. Avoid hot tubs and saunas. Limit hot showers to less than 15 minutes. Do not apply a heating pad or ice to swollen areas.
Know when to seek medical care. Call your health care team if you have any of the following signs of infection:
-
Temperature higher than 100.5 degrees Fahrenheit (38 degrees Celsius)
-
Skin that is hot to the touch
-
New areas of skin redness, swelling, or pain
Questions to ask the health care team
-
Am I at risk for developing lymphedema?
-
Is there anything I can do to prevent lymphedema?
-
What symptoms of lymphedema should I watch out for?
-
Are there signs that my lymphedema may be getting worse that I should tell you about?
-
Can you recommend a local certified lymphedema therapist?
-
What can I do at home to manage my lymphedema?
Related Resources
Leg Swelling After Cancer Treatment: What Can You Do?
Fear of Treatment-Related Side Effects
More Information
Lymphatic Education & Research Network
Lymphology Association of North America (LANA): Find a LANA Certified Therapist

 Download
Download