ON THIS PAGE: You will learn about the different types of treatments for cervical cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for cervical cancer. “Standard of care” means the best treatments known. Information in this section is based on medical standards of care for cervical cancer in the United States. Treatment options can vary from one place to another.
Clinical trials may also be an option for you, which is something you can discuss with your doctor. A clinical trial is a research study that tests a new approach to treatment. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How cervical cancer is treated
In cancer care, different types of doctors who specialize in cancer, called oncologists, often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. Cancer care teams include other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, physical therapists, occupational therapists, and others. Learn more about the clinicians who provide cancer care.
The treatment of cervical cancer depends on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of conversations are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is important for cervical cancer because there are different treatment options. Learn more about making treatment decisions.
A diagnosis of cervical cancer may bring concerns about if or how treatment may affect sexual function and the ability to have children, called fertility. These topics should be discussed with the health care team before treatment begins. If you are pregnant, talk with the doctor about your treatment options, including whether or not each could affect your unborn child. Treatment may be able to be delayed until after the baby is born.
The common types of treatments used for cervical cancer are described below. Your care plan may also include treatment for symptoms and side effects, an important part of cancer care.
READ MORE BELOW:
Surgery
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. For cancer that has not spread beyond the cervix, these procedures are often used:
-
Conization. The use of the same procedure as a cone biopsy (see Diagnosis) to remove all of the abnormal tissue. It can be used to remove cervical cancer that can only be seen with a microscope, called microinvasive cancer.
-
Loop electrosurgical excision procedure (LEEP). The use of an electrical current passed through a thin wire hook. The hook removes the tissue. It can be used to remove microinvasive cervical cancer.
-
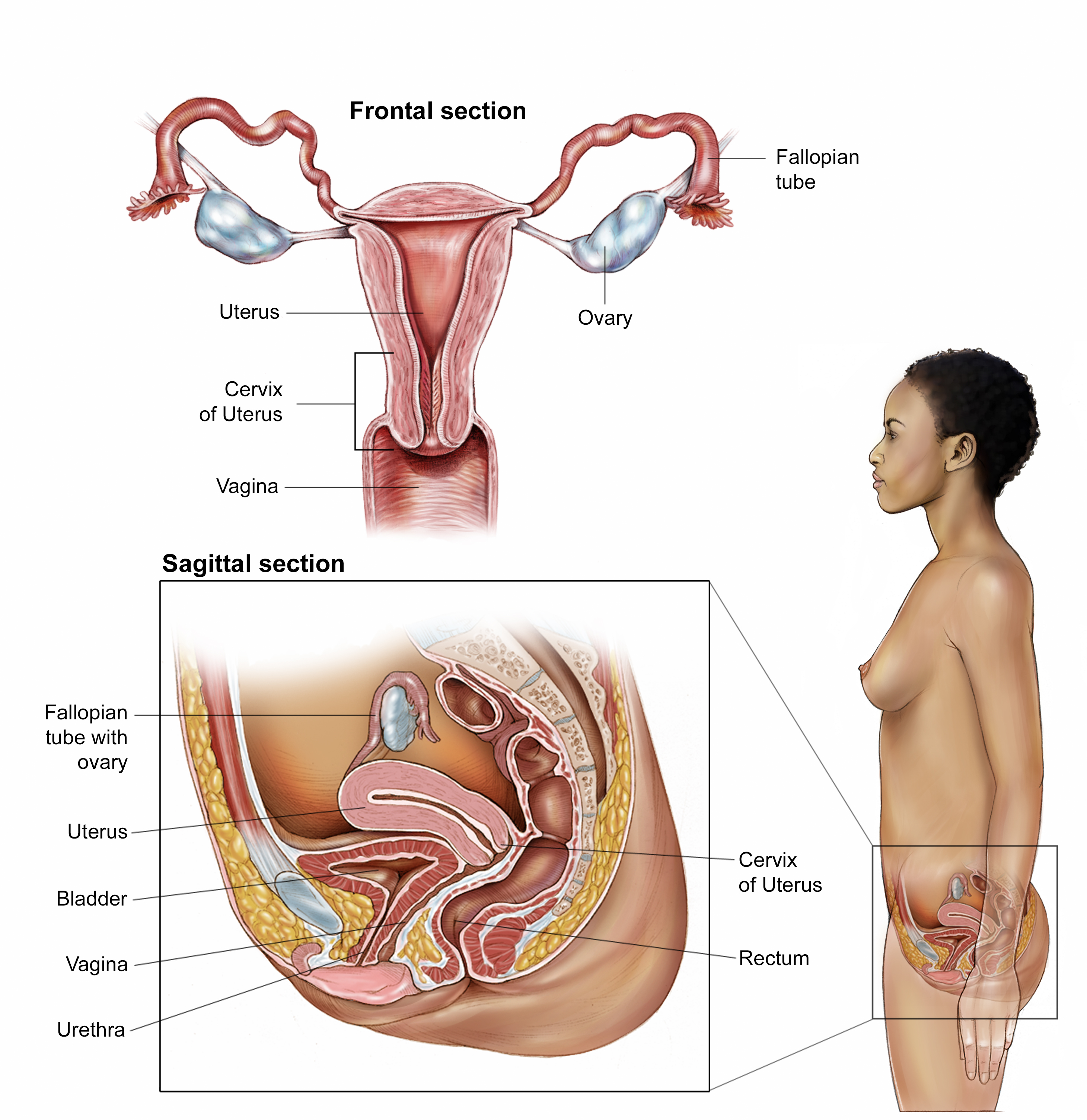
Hysterectomy. The removal of the uterus and cervix. A hysterectomy can be either simple or radical. A simple hysterectomy is the removal of the uterus and cervix. A radical hysterectomy is the removal of the uterus, cervix, upper vagina, and the tissue around the cervix. A radical hysterectomy also includes an extensive pelvic lymph node dissection, which means lymph nodes are removed. This procedure can be done using a large cut in the abdomen, called laparotomy, or using smaller cuts, called laparoscopy.
-
Bilateral salpingo-oophorectomy. If needed, this surgery is the removal of both fallopian tubes and both ovaries. It is done at the same time as a hysterectomy.
-
Radical trachelectomy. A surgical procedure in which the cervix is removed, but the uterus is left intact. It includes pelvic lymph node dissection (see above). This surgery may be used for young patients who want to preserve their fertility. This procedure has become an acceptable alternative to a hysterectomy for some patients.
-
Exenteration. The removal of the uterus, vagina, lower colon, rectum, or bladder if cervical cancer has spread to these organs after radiation therapy (see below). Exenteration is rarely recommended. It is most often used when cancer has come back after radiation therapy.
Complications or side effects from surgery vary depending on the type and extent of the procedure. Occasionally, patients experience significant bleeding, infection, or damage to the urinary and intestinal systems. Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have and how they can be relieved.
Because these surgical procedures affect sexual health, patients should talk with their doctor about their symptoms and concerns in detail before the surgery. The doctor may be able to help reduce the side effects of surgery and provide support resources on coping with any changes. If extensive surgical procedures have affected sexual function, other surgical procedures can be used to make an artificial vagina.
Learn more about the basics of cancer surgery.
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. Radiation therapy may be given alone, before surgery, or instead of surgery to shrink the tumor.
The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. When radiation treatment is given using implants, it is called internal radiation therapy or brachytherapy. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time that combines external and internal radiation treatments. This combined approach is the most effective to reduce the chances the cancer will come back, called a recurrence.
For early stages of cervical cancer, a combination of radiation therapy and low-dose weekly chemotherapy is often used (see below). The goal of radiation therapy combined with chemotherapy is to increase the effectiveness of the radiation treatment. This combination is given to control the cancer in the pelvis with the goal of curing the cancer without surgery. It may also be given to destroy microscopic cancer cells that might remain after surgery.
Side effects from radiation therapy may include fatigue, mild skin reactions, upset stomach, and loose bowel movements. Side effects of internal radiation therapy may include abdominal pain and bowel obstruction, although it is uncommon. Most side effects usually go away after treatment is finished. After radiation therapy, the vaginal area may lose elasticity, so some patients may also want to use a vaginal dilator, which is a plastic or rubber cylinder that is inserted into the vagina to prevent narrowing. People who have received external-beam radiation therapy will lose the ability to become pregnant, and unless the ovaries have been surgically moved out of the pelvis, premenopausal patients will enter menopause.
Sometimes, doctors advise their patients not to have sexual intercourse during radiation therapy. Normal sexual activity can restart within a few weeks after treatment if the patient feels ready.
Learn more about the basics of radiation therapy, or read the American Society for Radiation Oncology’s pamphlet, Radiation Therapy for Gynecologic Cancers (PDF; please note that this link takes you to a separate, external website).
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication, or a gynecologic oncologist. Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications to take at home, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for cervical cancer include:
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
Each of these types of therapies is discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or a combination of different drugs given at the same time. For people with cervical cancer, chemotherapy is often given in combination with radiation therapy (see above).
Although chemotherapy can be given orally (by mouth), all the drugs used to treat cervical cancer are given intravenously (IV). IV chemotherapy is either injected directly into a vein or given through a thin tube called a catheter, which is a tube temporarily put into a large vein to make injections easier.
The side effects of chemotherapy depend on the individual and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away after treatment is finished.
Rarely, specific drugs may cause some hearing loss. Others may cause kidney damage or peripheral neuropathy, which is numbness, pain, or tingling in the hands or feet. Patients may be given extra fluid intravenously to protect their kidneys. Talk with your doctor about the possible short-term and long-term side effects based on the drugs and dosages you will be receiving.
Learn more about the basics of chemotherapy.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them.
If cervical cancer comes back after treatment, called recurrent cancer, or if cervical cancer has spread beyond the pelvis, called metastatic disease, it can be treated with a platinum-based chemotherapy combined with the targeted therapy bevacizumab (Avastin). There are 2 drugs similar to bevacizumab, called bevacizumab-awwb (Mvasi) and bevacizumab-bvzr (Zirabev), that have been approved by the U.S. Food and Drug Administration (FDA) to treat advanced cervical cancer. These are called biosimilars.
In addition, in 2021, the FDA granted accelerated approval to the targeted therapy tisotumab vedotin (HuMax-TF) for the treatment of recurrent or metastatic cervical cancer that has progressed during or after chemotherapy. Tisotumab vedotin is a type of targeted therapy called an antibody-drug conjugate that works by attaching to targets on cancer cells and then releasing a small amount of the anticancer drug directly into the tumor cells.
Talk with your doctor about the possible side effects of the targeted therapy prescribed for you and how they can be managed. Learn more about the basics of targeted treatments.
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells.
The immune checkpoint inhibitor pembrolizumab (Keytruda) is used to treat cervical cancer that has recurred or spread to other parts of the body during or after treatment with chemotherapy. In those with newly diagnosed advanced cervical cancer, pembrolizumab may be combined with chemotherapy and radiation therapy as an initial treatment. Pembrolizumab may also be used in combination with chemotherapy with or without bevacizumab in people with recurrent or metastatic cervical cancer whose tumors express PD-L1. Some cancer cells express the PD-L1 protein, which binds to the PD-1 protein on T cells. T cells are immune system cells that kill certain other cells, like cancer cells. When the PD-1 and PD-L1 proteins bind, the T cell does not attack the cancer cell. Pembrolizumab is a PD-1 inhibitor, so it blocks the binding between PD-1 and PD-L1, which allows the T cells to find and attack the cancer cells.
Different types of immunotherapy can cause different side effects. Common side effects include skin reactions, flu-like symptoms, diarrhea, and weight changes. Talk with your doctor about possible side effects for the immunotherapy recommended for you. Learn more about the basics of immunotherapy.
Return to top
Physical, emotional, social, and financial effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative and supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative and supportive care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative and supportive care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments, such as chemotherapy, surgery, or radiation therapy, to improve symptoms.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative and supportive care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
Cancer care is often expensive, and navigating health insurance can be difficult. Ask your doctor or another member of your health care team about talking with a financial navigator or counselor who may be able to help with your financial concerns.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Return to top
Treatment options by stage
Radiation therapy alone or surgery is generally used for an early-stage tumor. These treatments have been shown to be equally effective at treating early-stage cervical cancer. Chemoradiation (a combination of chemotherapy and radiation therapy) is generally used for people with a larger tumor, an advanced-stage tumor found only in the pelvis, or if the lymph nodes have cancer cells. Commonly, radiation therapy and chemotherapy are used after surgery if there is a high risk of the cancer coming back or if the cancer has spread.
Return to top
Metastatic cervical cancer
If cancer spreads to another part in the body from where it started, doctors call it metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
Chemotherapy, immunotherapy, surgery, and targeted therapy may be used to treat or remove newly affected areas in both the pelvic area and other parts of the body. Palliative and supportive care will also be important to help relieve symptoms and side effects, especially to relieve pain and other side effects from radiation therapy.
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. An important part of follow-up care is watching for recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the cancer returns after the original treatment, it is called recurrent cancer. Recurrent cancer may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence).
If a recurrence happens, a new cycle of testing will begin to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, systemic therapy, and radiation therapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent cervical cancer. Whichever treatment plan you choose, palliative and supportive care will be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Return to top
If treatment does not work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called incurable, distant metastatic, or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
Planning for your future care and putting your wishes in writing is important, especially at this stage of disease. Then, your health care team and loved ones will know what you want, even if you are unable to make these decisions. Learn more about putting your health care wishes in writing.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with your doctor or a member of your palliative care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.