ON THIS PAGE: You will find basic information about this group of diseases and the parts of the body they may affect. This is the first page of Cancer.Net’s Guide to Gestational Trophoblastic Disease. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
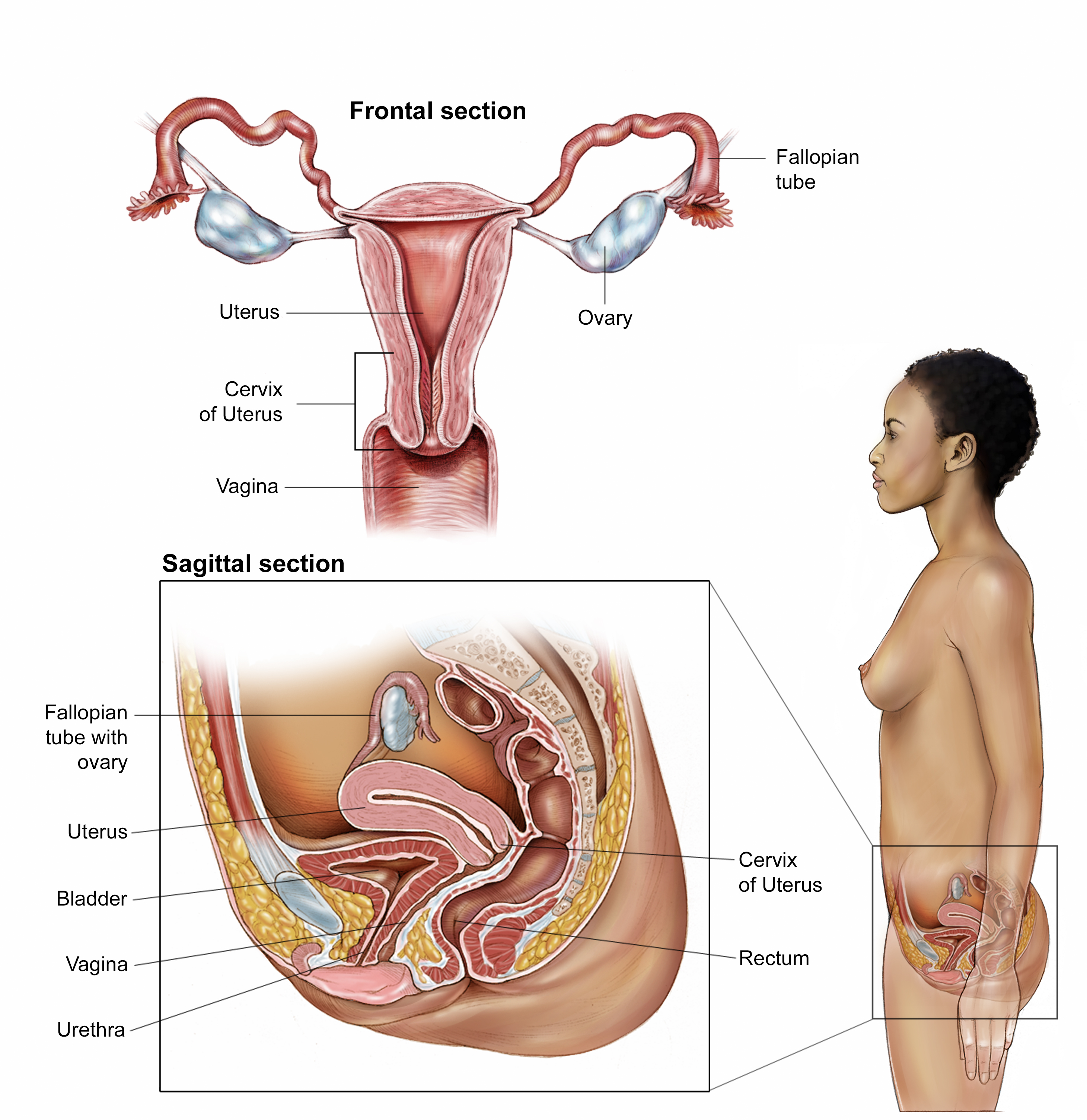
Gestational trophoblastic disease (GTD) affects the uterus. The uterus is a part of the female reproductive system. It is pear-shaped, hollow, and located in the pelvis between the bladder and rectum. The uterus is also known as the womb, where a fetus, or unborn baby, grows during pregnancy.
The uterus has 2 sections: the cervix, which is the narrow, lower section, and the corpus, which is the broad, middle section. The fundus is the dome-shaped top section of the corpus. The uterine wall has 2 layers of tissue. The inner layer is called the endometrium. The outer layer is muscle tissue called the myometrium. See the next section in this guide for illustrations of gynecologic anatomy.
About GTD
GTD is the general name for a group of rare tumors that can occur during pregnancy in the fetal chorion, which is the outer part of the sac that surrounds the fetus as it grows. GTD can occur during any pregnancy. GTD is almost always curable, especially if found early.
This type of tumor begins when normal cells of the placenta, called trophoblast cells, change and form a mass. GTD is usually benign, which means noncancerous. Some GTD tumors can be cancerous, also called malignant, meaning they can spread to other parts of the body.
Usually, GTD occurs when there is a problem during the combination of the sperm and the egg in the uterus. Trophoblast cells normally grow and surround a fertilized egg in the uterus, helping to connect the fertilized egg to the uterine wall and to form the placenta. The placenta is the organ that develops during pregnancy to provide nutrients to the fetus. But when this type of problem occurs in the tissues of the placenta, a healthy fetus usually does not develop. In rare cases, GTD is a cancerous growth that begins from a normal placenta, and it may be found after a normal pregnancy and birth of a baby.
Types of GTD
There are 2 main groupings of GTD. The first group is called molar pregnancy, also called hydatidiform moles. The second group is called gestational trophoblastic neoplasia (GTN). There are subtypes under each grouping, explained below.
Molar pregnancy (hydatidiform moles). Molar pregnancies account for about 80% of all GTD. There are 2 types of molar pregnancy: complete or partial. They are usually slow growing and benign, although there is a chance a mole can become cancerous. A complete molar pregnancy is much more likely to become cancerous than a partial molar pregnancy.
-
A complete molar pregnancy begins when sperm fertilizes an abnormal egg that doesn’t contain the mother’s DNA or a nucleus. There is no chance that a healthy baby will develop. Instead of forming a fetus, the tissue grows into a mound of cells that look like grape-shaped cysts. This may also be called a complete hydatidiform mole.
-
A partial molar pregnancy begins with the fertilization of a normal egg by 2 sperm, so there are 2 sets of DNA from the father. The result has some of the features of a complete molar pregnancy and part of the fetus may form, but there is no chance that a healthy baby will develop. This may also be called a partial hydatidiform mole.
GTN. While GTNs can be related to molar pregnancy, they are typically cancerous. This means they can spread to other parts of the body. The main types of GTNs include:
-
Invasive mole. Although an invasive mole is a type of molar pregnancy, it is considered a GTN because of its potential to grow and spread. An invasive mole may grow into the muscle layer of the uterus. Fewer than 15% of molar pregnancies become invasive and spread outside of the uterus.
-
Choriocarcinoma. This is a cancerous tumor formed from trophoblast cells. It can grow and spread more quickly than other GTNs. Choriocarcinoma can spread to the uterine muscle layer, nearby blood vessels, and outside of the uterus to nearby organs or to distant organs, like the brain, lungs, liver, or kidneys. About 5% of all GTD is choriocarcinoma. It is most often found in people who have had a molar pregnancy. Less often, choriocarcinoma occurs after a normal pregnancy, abortion, or tubal pregnancy, which is when the fetus grows in the fallopian tube instead of the uterus.
-
Placental-site trophoblastic tumor (PSTT). This rare type of GTN is also formed from trophoblast cells. It starts where the placenta joins with the uterus. This type of tumor grows slowly, but it can eventually spread to the uterine muscle, nearby blood vessels, and lymph nodes, pelvis, or lungs. Signs and symptoms may not occur until well after a normal pregnancy, an abortion, or treatment for a molar pregnancy.
-
Epithelioid trophoblastic tumor (ETT). This is an extremely rare type of GTD. If it does spread, the most common area of spread is to the lungs. It is most often found after a normal pregnancy and can take a long time to show signs and symptoms.
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
Find a Cancer Doctor. Search for a cancer specialist in your local area using this free database of doctors from the American Society of Clinical Oncology (ASCO).
-
Cancer Terms. Learn what medical phrases and terms used in cancer care and treatment mean.
The next section in this guide is Statistics. It helps explain the number of people who are diagnosed with GTD and their survival rates. Use the menu to choose a different section to read in this guide.