ON THIS PAGE: You will learn about the different types of treatments doctors use for people with prostate cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for prostate cancer. “Standard of care” means the best treatments known. When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials are an option. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How prostate cancer is treated
In cancer care, different types of doctors—including medical oncologists, surgeons, and radiation oncologists—often work together to create an overall treatment plan that may combine different types of treatments to treat the cancer. This is called a multidisciplinary team. Cancer care teams include a variety of other health care professionals, such as palliative care experts, physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, physical therapists, and others.
Treatment options and recommendations depend on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health.
Cancer treatment can affect adults who are 65 and older in different ways. More information on the specific effects of surgery, chemotherapy, and radiation therapy on these patients can be found another section of this website.
Take time to learn about your treatment options and be sure to ask questions if something is unclear. Talk with your doctor about the goals of each treatment, the likelihood that the treatment will work, what you can expect while receiving the treatment, and the possible urinary, bowel, sexual, and hormone-related side effects of treatment. Discuss with your doctor how the treatment options may affect recurrence, survival, and quality of life. It is also important to discuss your doctor's experience with treating prostate cancer. These types of talks are called "shared decision-making." Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is particularly important for prostate cancer because there are different treatment options. Learn more about making treatment decisions.
Because most prostate cancers are found in the early stages when they are growing slowly, you usually do not have to rush to make treatment decisions. During this time, it is important to talk with your doctor about the risks and benefits of all your treatment options and when treatment should begin. This discussion should also address the current state of the cancer:
-
Whether you have symptoms or prostate-specific antigen (PSA) levels are rising rapidly
-
Whether the cancer has spread to the bones
-
Your health history
-
Your quality of life
-
Your current urinary and sexual function
-
Any other medical conditions you may have
Although your treatment recommendations will depend on these factors, there are some general steps for treating prostate cancer by stage. These are described in "Treatments by stage of prostate cancer," further down this page.
The common types of treatments used for prostate cancer are described below. Your care plan may also include treatment for symptoms and side effects, an important part of cancer care.
Active surveillance and watchful waiting
If prostate cancer is in an early stage, is growing slowly, and treating the cancer would cause more problems than the disease itself, a doctor may recommend active surveillance or watchful waiting.
Active surveillance. Prostate cancer treatments may seriously affect a person's quality of life. These treatments can cause side effects, such as erectile dysfunction, which is the inability to get and maintain an erection of the penis, and incontinence, which is when urine flow or bowel function cannot be controlled. In addition, many prostate cancers grow slowly and cause no symptoms or problems. For this reason, many people may consider delaying cancer treatment rather than starting treatment right away. This is an approach called active surveillance. During active surveillance, the cancer is closely monitored for signs that it is worsening. If the cancer is found to be worsening, treatment will begin.
Active surveillance is usually preferred for those with very-low-risk and low-risk prostate cancer that can be treated with surgery or radiation therapy if it shows signs of getting worse. ASCO endorses recommendations from CancerCare Ontario on active surveillance, which recommend active surveillance for most patients with cancer that has not spread beyond the prostate, with a Gleason score of 6 or below. Sometimes, active surveillance may be an option for prostate cancer with a Gleason score of 7. There is also growing use of genomic testing to help find out if active surveillance is the best choice for a person with prostate cancer (see more in Latest Research).
ASCO encourages the following testing schedule for active surveillance:
-
A PSA test every 3 to 6 months
-
A digital rectam exam (DRE) at least once every year
-
Another prostate biopsy within 6 to 12 months, then a biopsy at least every 2 to 5 years
Treatment should begin if the results of the tests done during active surveillance show signs of the cancer becoming more aggressive or spreading, if the cancer causes pain, or if the cancer blocks the urinary tract.
Watchful waiting. Watchful waiting is an approach that may be an option for older adults and those with other serious or life-threatening illnesses who are expected to live less than 5 years. With watchful waiting, routine PSA tests, DRE, and biopsies are not usually done. If the prostate cancer causes symptoms, such as pain or blockage of the urinary tract, then treatment may be recommended to relieve those symptoms. This may include hormonal therapy (see below). Patients who start on active surveillance who later have a shorter life expectancy may switch to watchful waiting at some point to avoid repeated tests and biopsies.
Doctors must collect as much information as possible about the patient’s other illnesses and life expectancy to determine whether active surveillance or watchful waiting is appropriate for each person. In addition, many doctors recommend a repeat biopsy shortly after diagnosis to confirm that the cancer is in an early stage and growing slowly before considering active surveillance for someone who is otherwise healthy. New information is becoming available all the time, and it is important to discuss these issues with the doctor to make the best decisions about treatment. Learn more about ASCO’s endorsement of recommendations for active surveillance on a different ASCO website.
Return to top
Local treatments
Local treatments get rid of cancer from a specific, limited area of the body. Such treatments include surgery and radiation therapy. For early-stage prostate cancer, local treatments may get rid of the cancer completely. If the cancer has spread outside the prostate gland, other types of treatment (such as medications) may be needed to destroy cancer cells located in other parts of the body.
Surgery
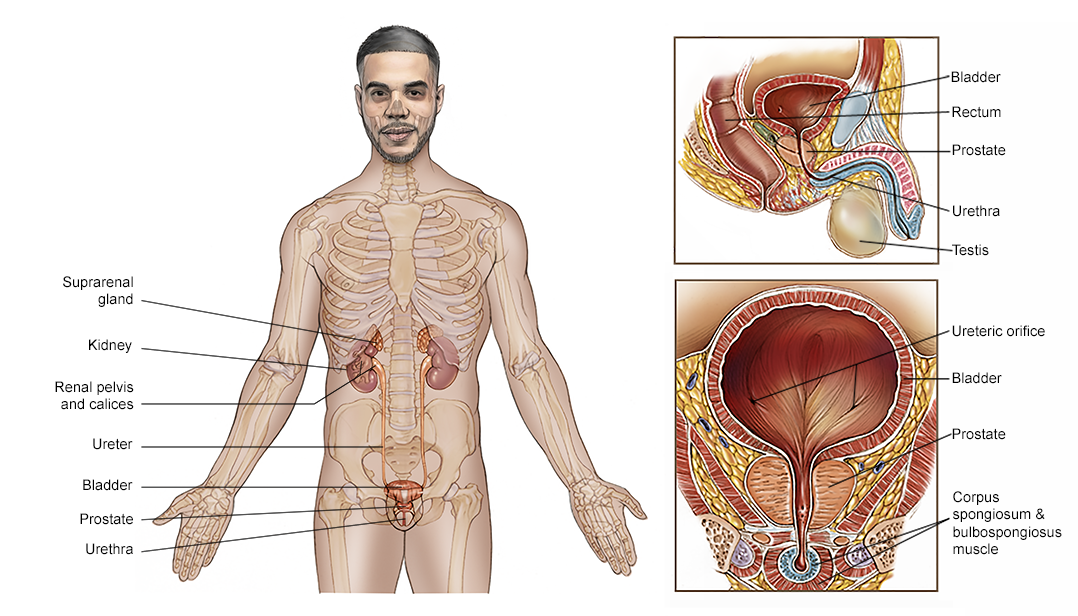
Surgery involves the removal of the prostate and some surrounding lymph nodes during an operation. A surgical oncologist is a doctor who specializes in treating cancer using surgery. For prostate cancer, a urologist or urologic oncologist is the surgical oncologist involved in treatment. The type of surgery depends on the stage of the disease, the patient’s overall health, and other factors.
-
Radical (open) prostatectomy. A radical prostatectomy is the surgical removal of the entire prostate and the seminal vesicles. Lymph nodes in the pelvic area may also be removed. This operation has the risk of affecting sexual function. Nerve-sparing surgery, when possible, increases the chance that the patient can maintain sexual function after surgery by avoiding surgical damage to the nerves that allow erections and orgasm to occur. Orgasm can occur even if some nerves are cut because these are separate processes. Urinary incontinence is also a possible side effect of radical prostatectomy. To help resume normal sexual function, drugs, penile implants, or injections may be recommended. Sometimes, another surgery can fix urinary incontinence.
-
Robotic or laparoscopic prostatectomy. This type of surgery is less invasive than a radical prostatectomy and may shorten recovery time. A camera and instruments are inserted through small keyhole incisions in the patient’s abdomen. The surgeon then directs the robotic instruments to remove the prostate gland. In general, robotic prostatectomy causes less bleeding and less pain, but the sexual and urinary side effects are similar to those of a radical (open) prostatectomy. Talk with your doctor about whether your treatment center offers this procedure and how it compares with the results of the radical (open) prostatectomy.
-
Bilateral orchiectomy. Bilateral orchiectomy is the surgical removal of both testicles. It is described in detail in “Hormonal therapy” below.
-
Transurethral resection of the prostate (TURP). TURP is most often used to relieve symptoms of a urinary blockage, not to treat prostate cancer. In this procedure, with the patient under full anesthesia, which is medication to block the awareness of pain, a surgeon inserts a narrow tube with a cutting device called a cystoscope into the urethra and then into the prostate to remove prostate tissue.
Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have. Typically, younger or healthier patients may benefit more from a prostatectomy. Younger patients are also less likely to develop permanent erectile dysfunction and urinary incontinence after a prostatectomy than older patients. Learn more about coping with the sexual side effects of prostate cancer in the Coping With Treatment section.
Learn more about the basics of cancer surgery.
Return to top
Radiation therapy
Radiation therapy is the use of high-energy rays to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
External-beam radiation therapy. External-beam radiation therapy is the most common type of radiation treatment. The radiation oncologist uses a machine located outside the body to focus a beam of x-rays on the area with the cancer.
One method of external-beam radiation therapy used to treat prostate cancer is called hypofractionated radiation therapy. This is when a person receives a higher daily dose of radiation therapy given over a shorter period, instead of lower doses given over a longer period. Extreme hypofraction radiation therapy is when the entire treatment is delivered in 5 or fewer treatments. Moderate hypofraction radiation therapy regimens typically include 20 to 28 treatments. This is also called stereotactic body radiation therapy (SBRT) or stereotactic ablative radiation therapy (SABR).
According to recommendations from ASCO, the American Society for Radiation Oncology, and the American Urological Association, hypofractionated radiation therapy may be an option for the following people with early-stage prostate cancer that has not spread to other parts of the body:
-
People with low-risk prostate cancer who need or prefer treatment instead of active surveillance.
-
People with intermediate-risk or high-risk prostate cancer receiving external-beam radiation therapy to the prostate and possibly the pelvic lymph nodes.
People who receive hypofractionated radiation therapy may have a slightly higher risk of some short-term side effects after treatment compared with those who receive regular external-beam radiation therapy. This may include gastrointestinal side effects. Based on current research, people who receive hypofractionated radiation therapy are not at a higher risk of side effects in the long term. Talk with your health care team if you have questions about your risk for side effects.
Learn more about these recommendations for hypofractionated radiation therapy for prostate cancer on a different ASCO website.
Brachytherapy. Brachytherapy, or internal radiation therapy, is the insertion of radioactive sources directly into the prostate. These sources, called seeds, give off radiation just around the area where they are inserted and may be left for a short time (high-dose rate) or for a longer time (low-dose rate). Low-dose-rate seeds are left in the prostate permanently and work for up to 1 year after they are inserted. However, how long they work depends on the source of radiation. High-dose-rate brachytherapy is usually left in the body for less than 30 minutes, but it may need to be given more than once.
Brachytherapy may be used with other treatments, such as external-beam radiation therapy and/or hormonal therapy. ASCO recommends the following brachytherapy options:
-
People with low-risk prostate cancer who need or choose an active treatment may consider low-dose-rate brachytherapy. Other options include external-beam radiation therapy or a radical prostatectomy.
-
People with intermediate-risk prostate cancer who choose external-beam radiation therapy (with or without hormonal therapy) should be offered either a low-dose-rate or high-dose-rate brachytherapy boost in addition to the external-beam radiation therapy. For a brachytherapy boost, a lower dose of radiation is given for a shorter period of time. Some patients with intermediate-risk prostate cancer may be able to receive only brachytherapy without external-beam radiation therapy or hormonal therapy.
-
Patients with high-risk prostate cancer who are receiving external-beam radiation therapy and hormonal therapy should be offered a low-dose-rate or high-dose-rate brachytherapy boost.
Read ASCO’s recommendations for brachytherapy for prostate cancer, found on a different ASCO website.
Intensity-modulated radiation therapy (IMRT). IMRT is a type of external-beam radiation therapy that uses computed tomography (CT) scans to form a 3D picture of the prostate before treatment. A computer uses this information about the size, shape, and location of the prostate cancer to determine how much radiation is needed to destroy it. With IMRT, high doses of radiation can be directed at the prostate without increasing the risk of damaging nearby organs.
Proton therapy. Proton therapy, also called proton beam therapy, is a type of external-beam radiation therapy that uses protons rather than x-rays. At high energy, protons can destroy cancer cells. Current research has not shown that proton therapy provides any more benefit to people with prostate cancer than traditional radiation therapy. It can also be more expensive.
Side effects of radiation therapy
Radiation therapy may cause side effects during treatment, including increased urge to urinate or frequency of urination; problems with sexual function; problems with bowel function, including diarrhea, rectal discomfort, or rectal bleeding; and fatigue. Most of these side effects usually go away after treatment.
To help support a patient's sexual functioning, drugs, penile implants, or injections may be recommended. Learn more about coping with the sexual side effects of prostate cancer in the Coping With Treatment section. While uncommon, some side effects of radiation therapy may not show up until years after treatment. See Follow-up Care for more information about long-term side effects.
Learn more about the basics of radiation therapy and what to expect when having radiation therapy.
Return to top
Focal therapies
Focal therapies are less-invasive treatments that destroy small prostate tumors without treating the rest of the prostate gland. These treatments use heat, cold, and other methods to treat cancer, mostly for low-risk or intermediate-risk prostate cancer. Focal therapies are being studied in clinical trials. Most have not been approved as standard treatment options.
Cryosurgery. Cryosurgery, also called cryotherapy or cryoablation, involves freezing cancer cells with a metal probe inserted through a small incision in the area between the rectum and the scrotum, the skin sac that contains the testicles. It is not an established therapy or standard of care to treat newly diagnosed prostate cancer. Cryosurgery has not been compared with radical prostatectomy or radiation therapy, so doctors do not know if it is a comparable treatment option. Its effects on urinary and sexual function are also not well known.
High-intensity focused ultrasound (HIFU). HIFU is a heat-based type of focal therapy. During HIFU treatment, an ultrasound probe is inserted into the rectum and then sound waves are directed at parts of the prostate gland with cancer. This treatment is designed to destroy cancer cells while limiting damage to the rest of the prostate gland. The FDA approved HIFU for the treatment of prostate tissue in 2015. HIFU may be an attractive option for some people, but knowing who may benefit most from this treatment is still unknown. HIFU should only be performed by a specialist with a lot of expertise. You will need to carefully discuss with your doctor if HIFU is the best treatment for you.
Return to top
Systemic treatments
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication.
Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for prostate cancer include:
Each of these types of therapies is discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications.
It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Androgen-deprivation therapy (hormonal therapy)
Because prostate cancer growth is driven by male sex hormones called androgens, lowering levels of these hormones can help slow the growth of the cancer. The most common androgen is testosterone. Androgen-deprivation therapy (ADT), or hormonal therapy, is used to lower testosterone levels in the body, either by surgically removing the testicles, known as surgical castration, or by taking drugs that turn off the function of the testicles, called medical castration. Which hormonal therapy is used is less important than the main goal of lowering testosterone levels.
Another way to stop testosterone from driving the growth of prostate cancer is to treat it with a type of medication called an androgen axis inhibitor. These medications can stop the body from making testosterone or stop testosterone from working. Androgen axis inhibitors include androgen receptor inhibitors and androgen synthesis inhibitors, which are both described in more detail below.
ADT is used to treat prostate cancer in many different situations, including localized, locally advanced, and metastatic prostate cancer, as well as rising PSA level after surgery and/or radiation therapy for localized prostate cancer. Some of the situations in which this therapy may be used include:
-
People with NCCN-based intermediate-risk and high-risk, localized prostate cancer who are having definitive therapy with radiation therapy are candidates for ADT. Definitive therapy is a treatment given with the intent to cure the cancer. People with intermediate-risk prostate cancer should receive ADT for at least 4 to 6 months. Those with high-risk prostate cancer should receive it for 2 to 3 years.
-
ADT may also be given to those who have had surgery and microscopic cancer cells were found in the removed lymph nodes. It is done to eliminate any remaining cancer cells and reduce the chance the cancer will return. This is known as adjuvant therapy. Although the use of adjuvant ADT is controversial, some specific patients appear to benefit from this approach.
Learn more about the basics of hormonal therapy.
Types of hormonal therapy for prostate cancer
Bilateral orchiectomy. Bilateral orchiectomy is the surgical removal of both testicles. It was the first treatment used for metastatic prostate cancer more than 70 years ago. Even though this is a surgical procedure, it is considered systemic hormonal therapy because it removes the main source of testosterone production: the testicles. The effects of this surgery are permanent and cannot be reversed. Bilateral orchiectomy is not commonly used anymore.
LHRH agonists. LHRH stands for luteinizing hormone-releasing hormone. Medications known as LHRH agonists prevent the testicles from receiving messages sent by the body to make testosterone. By blocking these signals, LHRH agonists reduce the testosterone level just as well as removing the testicles. Unlike orchiectomy, the effects of LHRH agonists are often reversible, so testosterone production usually begins again once treatment stops. However, testosterone recovery can take from 6 months to 24 months, and for a small number of patients, testosterone production does not return.
LHRH agonists are injected or placed as small implants under the skin. Depending on the drug used, they may be given once a month or once a year. When LHRH agonists are first given, testosterone levels briefly increase before falling to very low levels. This effect is known as a “flare.” Flares occur because the testicles temporarily release more testosterone in response to the way LHRH agonists work in the body. This flare may increase the activity of prostate cancer cells and cause symptoms and side effects, such as bone pain if the cancer has spread to the bone.
GnRH antagonist. GnRH stands for gonadotropin-releasing hormone. This class of drugs stops the testicles from producing testosterone like LHRH agonists, but they reduce testosterone levels more quickly and do not cause the flare associated with LHRH agonists. The U.S. Food and Drug Administration (FDA) has approved degarelix (Firmagon), given by monthly injection, to treat advanced prostate cancer. One side effect of this drug is that it may cause a severe allergic reaction. An oral GnRH antagonist, relugolix (Orgovyx), is also approved by the FDA for the treatment of advanced prostate cancer. Relugolix has a lower risk of causing serious heart problems in patients with preexisting heart disease. In addition, when treatment with relugolix is stopped, testosterone production is restored within weeks, rather than months, which may be helpful for those undergoing intermittent ADT (see below).
Androgen receptor (AR) inhibitors. While LHRH agonists and GnRH antagonists lower testosterone levels in the blood, androgen receptor (AR) inhibitors block testosterone from binding to so-called “androgen receptors,” which are chemical structures in cancer cells that allow testosterone and other male hormones to enter the cells. In effect, AR inhibitors stop testosterone from working. Newer AR inhibitors include apalutamide (Erleada), darolutamide (Nubeqa), and enzalutamide (Xtandi). Older AR inhibitors include bicalutamide (Casodex), flutamide (available as a generic drug), and nilutamide (Nilandron) and are taken as pills.
These medications are also sometimes called anti-androgens. AR inhibitors can be given to people who have “castration-sensitive” prostate cancer, which means that the prostate cancer still responds to treatments that lower testosterone levels. AR inhibitors are not usually used by themselves to treat prostate cancer.
-
Apalutamide. Apalutamide is approved by the FDA for the treatment of non-metastatic castration-resistant prostate cancer and for metastatic castration-sensitive prostate cancer in combination with ADT.
-
Darolutamide. Darolutamide is approved for the treatment of non-metastatic castration-resistant prostate cancer. It may also be used in combination with docetaxel chemotherapy to treat metastatic castration-sensitive prostate cancer.
-
Enzalutamide (updated 11/2023). Enzalutamide is a nonsteroidal AR inhibitor that is approved to treat metastatic and non-metastatic castration-resistant prostate cancer as well as metastatic and non-metastatic castration-sensitive prostate cancer.
Androgen synthesis inhibitors. Although the testicles produce most of the body's testosterone, other cells in the body can still make small amounts of the hormone that may drive cancer growth. These include the adrenal glands and some prostate cancer cells. Androgen synthesis inhibitors target an enzyme called CYP17 and stop cells from making testosterone.
-
Abiraterone acetate (Zytiga). Abiraterone acetate is taken in the form of a pill. Patients may take abiraterone with prednisone (multiple brand names) or prednisolone (multiple brand names). Prednisone or prednisolone helps prevent some of the side effects of abiraterone.
-
Ketoconazole (Nizoral). Ketoconazole is an androgen synthesis inhibitor that is no longer widely used because of multiple drug interactions. However, ketoconazole may be an option for some patients.
Combined androgen blockade. Sometimes androgen receptor inhibitors are combined with bilateral orchiectomy or LHRH agonist treatment to maximize the blockade of male hormones or to prevent the flare associated with treatment with LHRH agonists (see above).
Intermittent ADT. Traditionally, ADT was given for the patient’s lifetime. During the past 2 decades, researchers have studied the use of intermittent ADT, which is when therapy is given for specific times (most commonly 6 months) and then stopped temporarily to allow for testosterone levels to recover. For these patients, ADT is restarted when the PSA begins to rise again. When to restart therapy (that is, at which PSA levels) is still a topic of debate. Using ADT in this way may lower the side effects related to the lack of testosterone and improve a person’s quality of life. ASCO recommends this approach only for people with high-risk PSA recurrence (see below) and with no evidence of metastatic disease after radical prostatectomy and/or radiation therapy. However, intermittent ADT has not been studied with chemotherapy or newer hormonal treatments, such as abiraterone or enzalutamide, so ASCO cannot recommend intermittent ADT with them.
Side effects of hormonal therapy
These treatments will cause side effects that generally go away after treatment has finished, except in those who have had an orchiectomy. General side effects include:
-
Erectile dysfunction
-
Loss of sexual desire
-
Hot flashes with sweating
-
Gynecomastia, which is growth of breast tissue that sometimes can lead to discomfort
-
Depression
-
Cognitive dysfunction and memory loss
-
Heart problems and heart disease
-
Weight gain
-
Loss of muscle mass
-
Osteopenia or osteoporosis, which is thinning of bones
Learn more about coping with the sexual side effects of prostate cancer treatment in the Coping With Treatment section.
Although testosterone levels may recover after stopping treatment, some who have received LHRH agonists for many years may continue to have hormonal effects, even if they are no longer taking these drugs.
Another serious side effect of these treatments is the risk of developing metabolic syndrome. Metabolic syndrome is a set of conditions, such as obesity, high levels of blood cholesterol, and high blood pressure, that increases a person’s risk of heart disease, stroke, and diabetes. Currently, it is not certain how often this happens or exactly why it happens, but it is quite clear that patients who receive ADT have an increased risk of developing metabolic syndrome. The risk is increased even if temporary medical castration is used. Find out more about the symptoms of hormone deprivation and how to manage them.
The risks and benefits of treatment should be carefully discussed with your doctor. For people with metastatic prostate cancer, especially if it is advanced and causing symptoms, most doctors believe that the benefits far outweigh the risks of side effects. It is highly encouraged that people receiving ADT take steps that help manage or avoid possible side effects. These include getting regular exercise, quitting smoking, eating a balanced diet, making sure to get enough vitamin D and calcium, and receiving comprehensive, preventive cardiovascular follow-up care.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments.
Targeted therapy for prostate cancer includes:
-
Olaparib (Lynparza) (updated 06/2023). Olaparib is a type of targeted therapy called a PARP inhibitor. It is approved for patients with metastatic castration-resistant prostate cancer whose disease has continued to grow and spread during treatment with abiraterone and/or enzalutamide and who have DNA-repair gene defects, which may be inherited or in the tumor. DNA-repair gene defects make it harder for cancer cells to repair damaged DNA. Certain genes, such as BRCA1, BRCA2, and several others, are linked with DNA-repair gene defects, and the presence of any of these can allow treatment with olaparib. Olaparib may be combined with abiraterone when used to treat new-onset metastatic castration-resistant prostate cancer with a BRCA mutation.
-
Rucaparib (Rubraca). Rucaparib is another PARP inhibitor approved to treat metastatic castration-resistant prostate cancer in patients whose disease has not been stopped by treatment with abiraterone and/or enzalutamide and chemotherapy, and who have a BRCA1 or BRCA2mutation that is either inherited or in the tumor.
-
Talazoparib (Talzenna) (updated 07/2023). Talazoparib is also a PARP inhibitor. It prevents cancer cells from repairing DNA damage by targeting a pathway called homologous recombination repair or HRR. Talazoparib is combined with enzalutamide to treat metastatic castration-resistant prostate cancer, but the cancer cells must have a mutation in the HRR gene.
-
Niraparib plus abiraterone (Akeega) (updated 08/2023). Niraparib is a PARP inhibitor. When it is combined with abiraterone, it may be used to treat metastatic castration-resistant prostate cancer with a BRCA mutation.
One or more tests must be given to determine whether a patient may receive niraparib plus abiraterone, olaparib, or rucaparib:
-
Testing for an inherited, or germline, mutation after discussion with a genetic counselor
-
Genomic sequencing of tumor tissue
-
Genomic sequencing of the tumor DNA floating in the bloodstream
Genomic sequencing may be performed on tissue that was previously collected or on tissue from a new biopsy. Germline mutation testing alone identifies about half of the patients eligible for this treatment. People with metastatic prostate cancer who are considering targeted therapy are encouraged to talk with their doctors about all 3 tests mentioned above.
Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Return to top
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells.
Chemotherapy may help those with advanced or castration-resistant prostate cancer and those with newly diagnosed or castration-sensitive metastatic prostate cancer. A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time.
There are several standard drugs used for prostate cancer. In general, standard chemotherapy begins with docetaxel (Taxotere) combined with prednisone.
Recent research shows adding docetaxel to ADT in those with newly diagnosed or castration-sensitive metastatic prostate cancer significantly helps people live longer and stops the disease from growing and spreading.
Cabazitaxel (Jevtana) is approved to treat metastatic castration-resistant prostate cancer that has been previously treated with docetaxel. It is a type of chemotherapy called a microtubule inhibitor.
The side effects of chemotherapy depend on the individual, the type of chemotherapy received, the dose used, and the length of treatment, but they can include fatigue, sores in the mouth and throat, diarrhea, nausea and vomiting, constipation, blood disorders, nervous system effects, changes in thinking and memory, sexual and reproductive issues, appetite loss, pain, and hair loss. The side effects of chemotherapy usually go away after treatment has finished. However, some side effects may continue, come back, or develop later. Ask your doctor which side effects you may experience, based on your treatment plan. Your health care team will work with you to manage or prevent many of these side effects.
Learn more about the basics of chemotherapy.
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells.
For some people with castration-resistant metastatic prostate cancer who have no or very few cancer symptoms and generally have not had chemotherapy, vaccine therapy with sipuleucel-T (Provenge) may be an option.
Sipuleucel-T is adapted for each patient. Before treatment, blood is removed from the patient in a process called leukapheresis. Special immune cells are separated from the patient’s blood, modified in the laboratory, and then put back into the patient. At this point, the patient’s immune system may recognize and destroy prostate cancer cells. When this treatment is used, it is difficult to know if the treatment is working to treat the cancer because treatment with sipuleucel-T does not lead to lower PSA levels, shrinking of the tumor, or keeping the cancer from getting worse. However, results from clinical trials have shown that treatment with sipuleucel-T can lengthen lives by about 4 months in people with metastatic castration-resistant prostate cancer with few or no symptoms.
Different types of immunotherapy can cause different side effects. Common side effects include skin reactions, flu-like symptoms, diarrhea, and weight changes. Talk with your doctor about possible side effects for the immunotherapy recommended for you. Learn more about the basics of immunotherapy.
Return to top
Radiation therapy by infusion
Radium-223 (Xofigo). This treatment is a radioactive substance used to treat castration-resistant prostate cancer that has spread to the bone. Radium-223 is an alpha-emitter radionucleotide that mimics calcium and targets areas in the bone where the cancer is causing changes. This treatment delivers radiation particles directly to tumors found in the bone, limiting damage to healthy tissue, including the bone marrow, where normal blood cells are made. Radium-223 is given by intravenous injection (IV) once a month for 6 months. This treatment is given by a radiation oncologist or a nuclear medicine doctor. Your medical oncologist should continue to follow your progress during this treatment to make sure the treatment is helping and that any potential side effects are managed. Treatment with radium-233 does not dependably lower PSA, so patients should not expect to see big decreases in PSA levels during treatment and, in fact, often PSA levels may rise.
Some people should not receive this treatment, especially those who have prostate cancer that has spread to the liver and/or lungs and/or those with enlarged lymph nodes (3 cm or more in diameter). Radium-223 should not be used in combination with abiraterone and prednisone because that combination increases the risk of bone fractures. Discuss with your doctor whether this medication is an option for you.
Lutetium Lu 177 vipivotide tetraxetan (Pluvicto). This treatment, also called 177Lu-PSMA-617, targets a specific protein called PSMA (prostate-specific membrane antigen) that is highly expressed on prostate cancer cells, and it therefore delivers radiation directly to the cancer cells. It is approved for the treatment of people with metastatic castration-resistant prostate cancer who have already received an AR inhibitor and taxane chemotherapy, such as docetaxel. To receive this treatment, a special type of positron-emission tomography (PET) scan needs to confirm that the cancer cells express PSMA (see Diagnosis). The most common side effects of this treatment include fatigue, dry mouth, nausea, anemia, loss of appetite, and constipation.
Return to top
Bone-modifying drugs
Bone health is an important issue in the lives of people with prostate cancer. Osteopenia and osteoporosis are bone conditions that can be caused or worsened by hormonal therapy. Patients receiving ADT for non-metastatic prostate cancer should be evaluated for risk of fractures. The most common way to find a person’s risk is with a dual-energy X-ray absorptiometry (DEXA) scan to measure the strength of the bones. Patients who are found to be at high risk for a fracture should receive treatment to lower the risk. Bone-modifying drugs that can be used in this situation include denosumab (Prolia, Xgeva), zoledronic acid (Reclast, Zometa), alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and pamidronate (Aredia). These medications can have side effects, so talk with your doctor about when to take the medication and which would be best based on your situation.
Bone-modifying drugs have not been shown to prevent the spread of prostate cancer to the bone in patients who do not currently have evidence of bone metastases.
In patients with prostate cancer that has spread to the bone, there is always some risk of bone problems, such as fracture, pain, and spinal cord compression. These are called “skeletal-related events.” When prostate cancer has spread to bone and has also become resistant to ADT (see "Metastatic castration-resistant prostate cancer" below), bone-modifying drugs may be recommended to reduce the risk of these problems. Specifically, denosumab or zoledronic acid can be given once per month to reduce that risk.
A rare but serious possible side effect of bone-modifying drugs is osteonecrosis of the jaw. The symptoms of osteonecrosis of the jaw include pain, swelling, and infection of the jaw; loose teeth; and exposed bone. The most prominent risk factor for this side effect is the need for invasive dental work (for example, tooth extraction) in a person who is already receiving a potent bone-modifying drug such as denosumab or zoledronic acid. It is important to have a dental evaluation before starting these drugs in order to assess safety and address problem areas before starting a bone-modifying drug. If someone taking these drugs needs dental work, treatment should be stopped until the dental work is completed and the patient has healed. Learn more about dental health and cancer.
This information is based on an ASCO endorsement of the Cancer Care Ontario guideline, “Bone Health and Bone-targeted Therapies for Prostate Cancer.” Note that this link takes you to a different ASCO website.
Return to top
Physical, emotional, and social effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Return to top
Treatment by stage of prostate cancer
Different treatments may be recommended for each stage of prostate cancer. The general options by stage are described below. For more detailed descriptions, see “How prostate cancer is treated,” above. Your doctor will work with you to develop a specific treatment plan based on your specific diagnosis and needs. Clinical trials may also be a treatment option for each stage.
Early-stage prostate cancer (stages I and II)
Early-stage prostate cancer usually grows very slowly and may take years to cause any symptoms or other health problems, if it ever does at all. As a result, active surveillance or watchful waiting may be recommended. Radiation therapy (external-beam or brachytherapy) or surgery may also be suggested, as well as treatment in clinical trials. For those with a higher Gleason score, the cancer may be faster growing, so radical prostatectomy and radiation therapy are often recommended. Your doctor will consider your age and general health before recommending a treatment plan.
ASCO, the American Urological Association, American Society of Radiation Oncology, and the Society of Urologic Oncology recommend that patients with high-risk early-stage prostate cancer that has not spread to other areas of the body should receive radical prostatectomy or radiation therapy with ADT as standard treatment options.
Return to top
Locally advanced prostate cancer (stage III)
Locally advanced prostate cancer may be treated with external-beam radiation therapy and concurrent ADT or with surgery alone. ASCO recommends that doctors consider ADT to stop testosterone production plus abiraterone and prednisolone when patients can receive this approach. If abiraterone is not an option, combined androgen blockade using an AR inhibitor may be recommended. Treatments may be given in different combinations to stop the cancer from growing and spreading. Active surveillance is also an option. For those who have not received previous local treatment, including surgery, and who are unwilling or unable to receive radiation therapy, early (immediate) ADT may be offered.
It is widely accepted that at least 24 months of ADT is needed to control the disease, but 18 months may also be enough. For those who have a radical prostatectomy, radiation therapy is given after the surgery. This is called adjuvant or salvage radiation therapy. It is a standard of care for prostate cancer with extraprostatic extension, which is when the tumor has spread to nearby areas outside the prostate gland. Those with a high risk of bone fractures may be given a bone-modifying drug on an osteoporosis treatment dose and schedule (see "Bone-modifying drugs” above).
Watchful waiting may be considered for older adults who are not expected to live for a long time and whose cancer is not causing symptoms or for those who have another, more serious illness.
Return to top
Advanced prostate cancer (stage IV)
If cancer spreads to another part in the body from where it started, doctors call it metastatic cancer. High-risk or locally advanced prostate cancers have a higher chance of becoming metastatic cancer. If prostate cancer has a high risk of becoming metastatic or is already metastatic, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
For many people, a diagnosis of advanced cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
There is no cure for metastatic prostate cancer, but it is often treatable for quite some time. Many people outlive their prostate cancer, even those who have advanced disease. Often, the prostate cancer grows slowly, and there are now effective treatment options that extend life even further. In this way, it can be like living with a chronic disease like heart disease or diabetes, requiring ongoing treatment to minimize symptoms and maintain well-being.
Supportive, or palliative, care to help relieve symptoms and side effects is an important part of the care of advanced prostate cancer. Supportive care options include:
-
TURP to manage symptoms such as bleeding or urinary obstruction (see "Surgery").
-
Bone-modifying drugs may be used to strengthen bones, reduce the risk of bone fractures, and reduce the risk of skeletal-related events for prostate cancer that has spread to the bone (see "Bone-modifying drugs").
-
Intravenous radiation therapy with radium-223, strontium, and samarium can also help relieve bone pain (see "Radiation therapy").
-
Palliative radiation therapy to specific bone areas can also be used to reduce bone pain when medications do not help.
Researchers are using other methods to better understand metastatic prostate cancer and identify new treatment approaches. For example, the Metastatic Prostate Cancer Project allows people with metastatic prostate cancer to enroll themselves. Please note that the link above takes you to another, independent website.
Biochemical or PSA recurrence (updated 11/2023)
Many people treated with surgery or radiation therapy are cured. However, some will develop a biochemical recurrence (BCR). The main signs of BCR are rising PSA levels and no metastases in scans. This is why BCR is also called "PSA recurrence" or “rising PSA syndrome.” Whether someone has BCR depends on what the first treatment for prostate cancer was.
For those who received a radical prostatectomy, BCR is defined as a rising PSA level that reaches a value of 0.2 ng/mL or more. Radiation therapy may be a treatment option for certain patients with BCR after surgery. This treatment is called “salvage radiation therapy.” Several factors are considered when deciding who can be treated with salvage radiation therapy, including Gleason score, pathologic stage, how long it took for BCR to happen, PSA level after surgery, and changes in PSA over time, also known as “PSA doubling time.”
For people who received radiation therapy as the main treatment for prostate cancer, BCR is defined as a normal testosterone level and a PSA value more than 2.0 ng/mL plus the lowest PSA value reached after the treatment with radiation therapy (this is called “nadir PSA”). Treating BCR after radiation therapy is more difficult. Treatment options can include surgery, called “salvage radical prostatectomy,” or cryosurgery, called “salvage cryotherapy” (see “Focal therapies,” above). You are encouraged to discuss the treatment options with the health care team.
ADT may be recommended, especially if other local treatments are not possible. For individuals with a high risk of metastasis, treatment with enzalutamide may be an option, regardless of whether the cancer was treated with prostatectomy or radiation therapy. If ADT is going to be used alone to treat the BCR, intermittent ADT may be an option.
Metastatic castration-sensitive prostate cancer (Updated 04/2023)
Prostate cancer that has spread to other parts of the body and still responds to treatment that suppresses testosterone is called metastatic castration-sensitive prostate cancer. The best treatment option depends on the patient's health and the extent of the cancer. It is important to talk with the health care team about the risks and benefits of each option. Some of the following treatment options can only be used to treat people who are newly diagnosed. Others can be used to treat those who have received previous treatments, including radical prostatectomy (surgery) or radiation therapy.
For people who have newly diagnosed metastatic prostate cancer and who will be receiving chemotherapy with docetaxel, treatment options include:
-
ADT plus docetaxel and darolutamide (triplet therapy). In people with newly diagnosed metastatic prostate cancer, who were starting docetaxel plus ADT, research has shown that adding darolutamide to the regimen helps people live longer. If a patient is starting treatment with docetaxel plus ADT, ASCO recommends adding darolutamide to the regimen. This only applies to those who are receiving docetaxel chemotherapy.
-
ADT plus docetaxel plus abiraterone with prednisone or prednisolone (triplet therapy). In people with high-volume, newly diagnosed metastatic prostate cancer who were starting docetaxel plus ADT, research has shown that adding abiraterone to the regimen helps people live longer. If a patient is starting treatment with docetaxel plus ADT, ASCO recommends adding abiraterone to the regimen. This only applies to those who are receiving docetaxel chemotherapy.
-
ADT plus docetaxel. This treatment is reserved for those who are newly diagnosed and able to receive chemotherapy but who are unable to receive abiraterone. Docetaxel with or without ADT is given by IV every 3 weeks for a total of 6 doses.
For people with newly diagnosed, high-risk prostate cancer who are not candidates for chemotherapy, ASCO recommends the following treatment:
For people with newly diagnosed metastatic prostate cancer, regardless of how much the disease has spread, and who are not starting docetaxel chemotherapy, ASCO recommends the following treatments:
-
ADT plus enzalutamide or ADT plus apalutamide. These 2 treatment options are recommended as options for patients with metastatic castration-sensitive prostate cancer. These options are available even if the patient has already been treated with surgery, radiation therapy, or ADT.
In addition to the above treatment options, treatment to relieve symptoms and side effects continues to be an important part of the overall treatment plan.
This information is based in part on the ASCO guideline, “Initial Management of Noncastrate Advanced, Recurrent, or Metastatic Prostate Cancer.” Note that this link takes you to a different ASCO website.
A bone-modifying drug may be recommended to prevent bone fractures (see "Bone-modifying drugs” above).
Non-metastatic castration-resistant prostate cancer
Prostate cancer that is no longer stopped by low testosterone levels (less than 50 ng/mL) is called “castration resistant.” Castration-resistant prostate cancer is defined by a rising PSA level and/or worsening symptoms and/or growing cancer verified by scans. If the cancer has not spread to other parts of the body, it is called “non-metastatic castration-resistant prostate cancer.”
ASCO recommends that treatment for non-metastatic castration-resistant prostate cancer should continue to focus on lowering testosterone levels. This may include a permanent treatment, such as orchiectomy, or it may include continuing treatment with medications that lower hormone levels, such as apalutamide, darolutamide, or enzalutamide.
For those who have not had chemotherapy, additional ADT may be an option if there is a high risk that the disease will spread. Talk with your doctor about your personal risk level.
PSA testing and/or imaging tests may be done regularly to see if the cancer has worsened or spread. If there is a low risk of developing metastatic disease, ASCO recommends PSA testing every 4 to 6 months. If there is a high risk of metastatic disease, ASCO recommends PSA testing every 3 months. Imaging tests, such as a bone scan, CT scan, or magnetic resonance imaging (MRI), may be done if there are symptoms or signs that the cancer is worsening.
Metastatic castration-resistant prostate cancer (updated 07/2023)
If the cancer is no longer stopped by low testosterone levels (less than 50 ng/mL) and has spread to other parts of the body, it is called “metastatic castration-resistant prostate cancer.” Castration-resistant prostate cancer is defined by a rising PSA level and/or worsening symptoms and/or growing cancer verified by scans. ASCO recommends PSA testing every 3 months for metastatic castration-resistant prostate cancer. Generally, imaging tests, such as CT scan and bone scan, are done to check the growth and spread of cancer and to see how well treatment is working.
Metastatic castration-resistant prostate cancer can be difficult to treat. ASCO recommends continuing treatment that lowers hormone levels for metastatic castration-resistant prostate cancer. ASCO has treatment recommendations for hormone therapy for advanced cancer and for systemic treatment of metastatic castration-resistant prostate cancer.
Treatment options for metastatic castration-resistant prostate cancer are listed below. Treatment in a clinical trial may also be an option.
-
AR inhibitors, such as abiraterone or enzalutamide
-
Targeted therapy with olaparib or rucaparib
-
AR inhibitor combined with a PARP inhibitor
-
Chemotherapy with docetaxel, especially if there is bone pain or other cancer-related symptoms
-
Chemotherapy with cabazitaxel if docetaxel stops working
-
Immunotherapy with sipuleucel-T
-
Radioligand therapy (targeted radiation therapy by infusion) using 177Lu-PSMA-617
-
Radium-223, a form of radiopharmaceutical therapy (non-targeted radiation therapy by infusion)
-
Bone-modifying drugs to treat cancer that has spread to the bone
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission can be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. Although there are treatments to help prevent a recurrence, such as hormonal therapy and radiation therapy, it is important to talk with your doctor about the possibility of the cancer returning. There are tools your doctor can use, called nomograms, to estimate someone's risk of recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
In general, following surgery or radiation therapy, the PSA level in the blood usually drops. If the PSA level starts to rise again, it may be a sign that the cancer has come back. If the cancer returns after the original treatment, it is called recurrent cancer.
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it, including where the recurrence is located. The cancer may come back in the prostate (called a local recurrence), in the tissues or lymph nodes near the prostate (a regional recurrence), or in another part of the body, such as the bones, lungs, or liver (a distant or metastatic recurrence). Sometimes the doctor cannot find a tumor even though the PSA level has increased. This is known as a PSA recurrence or biochemical recurrence (BCR).
After this testing is done, you and your doctor will talk about the treatment options. The choice of treatment plan is based on the type of recurrence and the treatment(s) you have already received and may include the treatments described above, such as radiation therapy, prostatectomy for people first treated with radiation therapy, or ADT. Your doctor may suggest clinical trials that are studying new ways to treat recurrent prostate cancer.
Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects. Palliative care usually includes pain medication, external-beam radiation therapy, brachytherapy with radium-223, strontium, or samarium, or other treatments to reduce bone pain.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Return to top
If treatment does not work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer may be difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment, including a hospital bed, can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.