ON THIS PAGE: You will learn about the different types of treatments doctors use for people with testicular cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for testicular cancer. “Standard of care” means the best treatments known. When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials are an option. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How testicular cancer is treated
In cancer care, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. For testicular cancer, this team includes a urologist and a medical oncologist. A medical oncologist is a doctor who specializes in treating cancer with medication. Sometimes, patients may also see a radiation oncologist. A radiation oncologist is a doctor who specializes in giving radiation therapy to treat cancer. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health. The first treatment for testicular cancer is usually surgery to remove the testicle. In rare cases, chemotherapy is given first if the cancer has already spread beyond the testicle when diagnosed and the patient's condition is unstable and requires urgent treatment of the metastatic disease.
After surgery, chemotherapy or radiation therapy may be recommended. Germ cell tumors are highly sensitive to chemotherapy and are usually curable even if the cancer has spread. But chemotherapy is not very effective for a specific type of germ cell tumor called a teratoma. This type needs to be removed with surgery. Because many non-seminomas are a mixture of teratoma and other types of germ cell tumor, successful treatment often requires chemotherapy followed by surgery to remove any of the remaining tumor.
Radiation therapy may be recommended to treat early-stage seminoma or cancer that has spread to the brain.
People with testicular cancer usually have concerns about how their treatment will affect their sexual health and fertility, as well as their quality of life. Discuss these topics with your doctor before treatment begins because there is often more than 1 treatment option available. The final choice of a treatment plan depends on your specific situation.
Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of talks are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Learn more about making treatment decisions.
The common types of treatments used for testicular cancer are described below, followed by treatment options by the cancer’s stage. Your care plan may also include treatment for symptoms and side effects, an important part of cancer care.
Physical, emotional, and social effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Return to top
Surgery
Surgery for cancer involves the removal of the tumor and, sometimes, some surrounding healthy tissue during an operation. For testicular cancer, the diagnosis is most often made by removing the cancerous testicle through an incision in the groin. This is called a radical inguinal orchiectomy. In addition to a radical orchiectomy, other types of surgery may be done for testicular cancer at different times in the treatment schedule. Each of these types of surgery is described below. Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have. Learn more about the basics of cancer surgery.
Radical inguinal orchiectomy
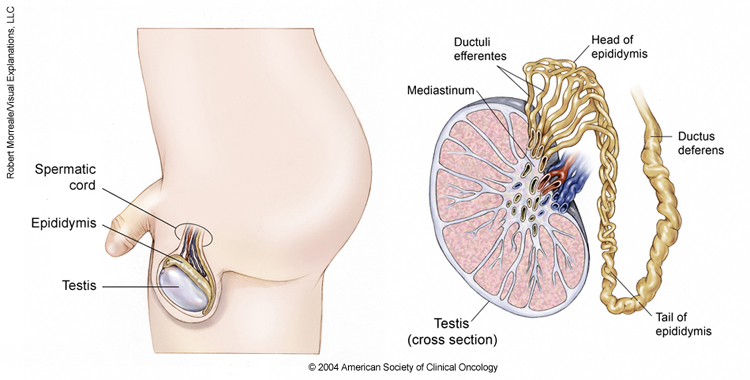
Treatment of testicular cancer usually starts with surgery to remove the testicle with cancer, called a radical inguinal orchiectomy. This operation is done through an incision in the groin along the beltline. During the surgery, the entire testicle and most of the spermatic cord are removed. The spermatic cord contains the blood supply to the testicle and the channel through which sperm travel from the testicle toward the penis.
Cancer may develop in both testicles at the same time or at different times. However, this is rare, occurring in about 2% of people with testicular cancer. Then, both testicles usually need to be removed in a procedure called a bilateral orchiectomy. In some cases where testicular cancer is in both testicles, testicle-sparing surgery can be performed on one side so that part of 1 testicle remains, but this is not commonly done.
Orchiectomy is used to diagnose and treat both early-stage and later-stage seminoma and non-seminoma. For later-stage cancer, a radical inguinal orchiectomy may, occasionally, not be done until treatment with chemotherapy has finished (see "Chemotherapy," below).
If a decision is made to perform an orchiectomy, a sample of blood will be collected before surgery to test for levels of serum tumor markers because they are often helpful in planning treatment and follow-up care. (See Diagnosis for more information about serum tumor markers.) For example, increasing or consistently high alpha-fetoprotein (AFP) or beta human chorionic gonadotropin (beta-hCG) after surgery is a sign that the cancer has spread. In this situation, a patient usually needs chemotherapy (see below), even if the metastases cannot be seen on imaging tests.
Side effects of orchiectomy
The removal of 1 testicle usually does not affect the body's testosterone level if there is still another testicle and it is normal size. When testosterone level is reduced, symptoms may include depression or other mood changes, fatigue, decreased sex drive, inability to achieve a normal erection, and hot flashes, as well as loss of muscle and bone mass in the long term. People with low testosterone levels after orchiectomy can be treated with supplemental testosterone.
Orchiectomy is unlikely to make someone unable to produce a biological child because the remaining testicle will still produce sperm. However, about 25% of people with testicular cancer are infertile even before they are diagnosed with cancer. It appears that the cancer itself and/or factors that contributed to the development of the cancer may cause some people to become infertile. Sperm counts often improve after the testicle with cancer is removed.
If both testicles are removed, the body will no longer produce sperm or testosterone and the person will not be able to biologically produce children. If the doctor recommends removing both testicles or the testicle in someone with 1 testicle, semen is usually analyzed before surgery to evaluate sperm count and function. If adequate numbers of functional sperm are present, then sperm banking is usually recommended, so that producing children in the future may be a possibility. In addition, testosterone replacement therapy will be needed if both testicles are removed. Learn more about preserving fertility and sexual health.
Reconstructive surgery after orchiectomy
Patients can decide if they want an artificial or prosthetic testicle implanted in the scrotum. A prosthetic testicle generally has a weight and texture that is similar to a normal testicle but not exactly the same. Some people find that a prosthetic testicle is uncomfortable, and some prefer not to have one at all. You are encouraged to talk with your doctor about whether you want one and the best timing for this implantation, if wanted. Some people prefer to wait until after the active treatment period is over to give this option full consideration.
Surveillance after orchiectomy
After having a radical inguinal orchiectomy, an option for people with clinical stage I testicular cancer (seminoma or non-seminoma) may be surveillance. The advantage of surveillance is that patients may avoid additional treatment that may not be needed. With surveillance, the patient is monitored closely, and active treatment begins only if the cancer recurs. This option involves regular doctor appointments for physical examinations, blood tests for tumor markers, computed tomography (CT) scans, and chest x-rays. This approach requires dedication by the doctor and patient to stick to the surveillance schedule so that any recurrence can be detected at an early stage. It is only considered as an option if AFP and beta-hCG levels are normal or return to normal after the testicle with cancer is removed.
The main advantage of surveillance is that it avoids any further treatment after orchiectomy — such as chemotherapy, radiation therapy, or additional surgery — for the 82% of patients with seminoma and 75% of patients with non-seminoma who will not have the disease return after orchiectomy. For an individual patient, the risk of recurrence may be higher or lower based on risk factors determined by the pathologist’s examination of the tumor after the testicle has been removed.
Retroperitoneal lymph node dissection (RPLND)
This is surgery to remove the retroperitoneal lymph nodes, which lie at the back of the abdomen in front of the spine. RPLND is usually performed as an open operation with an incision, or cut, down the middle of the abdomen. RPLND is a complex surgery requiring experience and skill to remove all of the appropriate lymph nodes and to lessen the side effects of the operation. RPLND should only be done by a surgeon who is highly experienced with this operation. Some surgeons perform laparoscopic RPLND, which uses several smaller incisions instead of the 1 large incision, but that approach is still being studied, requires a surgeon skilled in the procedure, may not be as effective, and may have risks.
Read below to learn more about when RPLND may be used.
RPLND for stage I and IIA non-seminoma
RPLND as a main treatment for stage I and stage IIA non-seminoma helps reduce the risk of recurrence and is used to stage the cancer. About 25% of patients with clinical stage I non-seminoma who have an RPLND are found to have lymph nodes with cancer, which means they have stage II disease. Doctors are now able to better determine which stage I tumors are more likely to have spread to the lymph nodes or beyond, based on the results of the pathology tests performed on the tumor in the testicle after it is removed. Decisions about whether to have an RPLND may be based on the patient’s risk factors. RPLND is a reasonable treatment option when a patient can see a urologist with extensive experience with RPLND. If an RPLND is chosen for stage I non-seminoma, it is usually done within 6 weeks after orchiectomy.
If 5 or fewer lymph nodes have cancer and none is larger than 2 cm (pN1), this surgery alone is successful for 80% to 90% of patients, while about 10% to 20% of patients will have a recurrence. If more lymph nodes have cancer (pN2 or pN3), surgery alone is successful for about 50% of patients, while the other 50% will have a recurrence. The advantage of the RPLND is that it can cure most patients with small amounts of cancer in the lymph nodes, provide a more accurate assessment of the extent of disease, and avoid the need for frequent CT scans of the abdomen during follow-up care. It also reduces the chance that someone with early-stage (stage I) testicular cancer will need chemotherapy.
Just as RPLND may show cancer in lymph nodes that appeared normal on CT scans for people with clinical stage I non-seminoma, surgery may also show that there is no cancer in lymph nodes that were enlarged on a CT scan, called clinical stage II disease. For people with clinical stage IIA testicular non-seminomas, as many as 20% to 30% will actually have pathological stage I cancer, meaning that the cancer has not spread to any lymph nodes. In these situations, RPLND can help avoid unnecessary chemotherapy.
The main disadvantage of this surgery for stage I non-seminoma is that 70% of patients are cured by removing the testicle. For these patients, a RPLND offers no curative benefit, although it does allow the patient to avoid regular CT scans and may offer peace of mind.
Despite the surgery, about 10% of testicular cancers come back even if the lymph nodes were not found to have cancer. If lymph nodes with cancer are found during the RPLND, 2 courses of chemotherapy (see below) can help lower the chance of recurrence to about 1%. However, surveillance is also an option, beginning treatment with chemotherapy only if the cancer recurs. This is because this type of testicular cancer has a greater than 90% chance of being cured with 3 cycles of chemotherapy if the recurrence is diagnosed early through regular monitoring. A study that compared chemotherapy to surveillance for men who had cancer in lymph nodes removed by RPLND found that there was no difference in survival, but chemotherapy did reduce the risk of the cancer coming back. In practice, most centers recommend surveillance after RPLND for pathological stage IIA disease, and chemotherapy after RPLND for pathological stage IIB and IIC disease.
RPLND to remove residual tumors after chemotherapy in patients with non-seminomas
RPLND is recommended for people with stage II or stage III non-seminoma who have retroperitoneal masses that remain after finishing chemotherapy (see below). In people with non-seminoma, any masses larger than 1 cm that remain after chemotherapy are removed, if it is possible. About 35% to 50% of patients having an RPLND will have a mass that contains teratoma. About 10% to 15% will have 1 of the other types of germ cell cancers. The other 35% to 50% will have no cancer or teratoma found and there will only be scarring and/or normal lymph node tissue.
Most experts believe that RPLND after chemotherapy is only needed if there are lymph nodes larger than 1 cm seen on scans taken after chemotherapy ends. However, some treatment centers will perform an RPLND after chemotherapy in those who had enlarged retroperitoneal lymph nodes before chemotherapy, even if the lymph nodes return to less than 1 cm after chemotherapy.
Treatment after post-chemotherapy RPLND depends on what is found at surgery. If only teratoma or benign tissue is found, no additional treatment is given after RPLND. If surgery reveals seminoma, embryonal carcinoma, yolk sac tumor, or choriocarcinoma, 2 additional cycles of chemotherapy are generally recommended after RPLND.
RPLND for stage I and IIA pure seminoma
Historically, RPLND has not been done as primary treatment for seminomas. Recently, a number of centers have been investigating RPLND for clinical stage II seminomas with the goal of sparing patients from undergoing chemotherapy or radiation therapy. However, this approach remains experimental while the results of such treatment are studied. The results thus far indicate that a majority of patients may be cured with RPLND and thus avoid chemotherapy and radiation, but the recurrence rates have been higher than the recurrence rates after chemotherapy or radiation therapy, and we do not yet have long-term follow-up. It is possible that recurrence rates after RPLND will rise with longer follow-up.
RPLND to remove residual tumors after chemotherapy in patients with seminomas
Masses smaller than 3 cm are usually left in place and monitored for changes with CT scans. Patients with pure seminoma who have masses larger than 3 cm after chemotherapy may also have CT scans to monitor the masses for growth. An alternative for patients with masses 3 cm or larger is to get an FDG PET-CT scan after chemotherapy and use the results of the PET scan to guide the treatment plan. If masses light up on the PET scan, surgery is generally used to find out whether the masses contain cancer. Sometimes, residual masses may light up on a PET scan but turn out not to have any cancer when they are removed surgically or biopsied. Therefore, different experts have different opinions on the usefulness of PET scans in this setting.
Side effects of RPLND
Some patients may experience temporary side effects from RPLND, such as bowel obstruction (blockage) or infection. This procedure should not affect the ability to have an erection, orgasm, or sexual intercourse. However, it may cause infertility because it can damage the nerves that control ejaculation, which can cause the inability to ejaculate. RPLND performed after chemotherapy is a more complex surgery and is more likely to cause the loss of ejaculation and other side effects.
Patients are encouraged to consider banking sperm before RPLND for fertility preservation. There are surgical techniques that are usually successful at sparing the nerves involved with ejaculation when RPLND is done as the initial treatment for stage I or stage II cancer. However, these techniques are much less effective when RPLND is done to remove residual masses after chemotherapy. Talk about these concerns with your doctors before surgery.
Other types of surgery to remove cancer remaining after chemotherapy
After chemotherapy (see below), some cancer may still remain in the lungs, liver, or other organs or in the lymph nodes in the pelvis, chest, or neck. For people with non-seminoma, these tumors should also be removed if it is safe to do so. This may involve surgery in more than 1 part of the body. This type of surgery is complex and requires an experienced team of surgeons. If only some of the remaining tumors can be removed, then surgery may not be performed.
Return to top
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. Chemotherapy is given by a medical oncologist, a doctor who specializes in treating cancer with medication.
Chemotherapy for testicular cancer is given directly into a vein so that it enters the bloodstream and reaches cancer cells throughout the body. There are also types of chemotherapy that can be taken by mouth, but they are not generally used for testicular cancer.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles of treatment given over a set period of time. A cycle of chemotherapy for testicular cancer typically lasts 3 weeks. Testicular cancer may be treated with 1 to 4 cycles of chemotherapy, depending on the stage of the cancer. During treatment, a patient may receive 1 drug at a time or a combination of different drugs given at the same time.
The following drugs are used for testicular cancer, usually in the combinations listed further below. However, the drugs used for testicular cancer change, and drugs other than those mentioned below may be used. Talk with your doctor about your options for chemotherapy.
-
Bleomycin (available as a generic drug)
-
Carboplatin (available as a generic drug)
-
Cisplatin (available as a generic drug)
-
Etoposide (available as a generic drug)
-
Gemcitabine (Gemzar)
-
Ifosfamide (Ifex)
-
Oxaliplatin (Eloxatin)
-
Paclitaxel (available as a generic drug)
-
Vinblastine (available as a generic drug)
The following chemotherapy regimens may be used for testicular cancer.
-
BEP: bleomycin, etoposide, and cisplatin
-
Carboplatin (for stage I pure seminoma only)
-
EP: etoposide and cisplatin
-
TIP: paclitaxel, ifosfamide, and cisplatin
-
VeIP: vinblastine, ifosfamide, and cisplatin
-
VIP: etoposide, ifosfamide, and cisplatin
-
High-dose carboplatin and etoposide
-
Gemcitabine, paclitaxel, and oxaliplatin
In general, later-stage disease is treated with more chemotherapy. The appropriate chemotherapy regimen depends on the stage of the cancer, whether it is a seminoma or a non-seminoma, and whether chemotherapy has previously been used to treat the cancer. In addition, how high AFP and beta-hCG levels are helps the doctor determine how much chemotherapy is needed. Chemotherapy regimens for specific stages are discussed further below.
Learn more about the basics of chemotherapy.
Side effects of chemotherapy
Chemotherapy works very well for testicular cancer but can cause side effects and complications. Common side effects from chemotherapy include fatigue, nausea and vomiting, numbness and tingling in the hands and feet, high-pitch hearing loss, and ringing in the ears. There is also a risk of severe infections, so you should talk with your health care team about what you should do if you develop symptoms of infection. The drug bleomycin is linked with dangerous inflammation in the lungs, so it is important to tell your health care team immediately if you have shortness of breath, difficulty breathing, or a persistent cough. People who received treatment for testicular cancer also have a higher risk of blood clots, particularly when they start treatment with chemotherapy. Tell your health care team right away if you have any signs of a blood clot, such as shortness of breath, chest pain, or swelling in 1 or both legs or arms.
Most side effects from chemotherapy usually go away after treatment is finished, but some can show up much later. These are called late effects. Late effects from chemotherapy for testicular cancer include long-lasting fatigue, heart disease, and second cancers. Recent data indicates that people with testicular cancer who are treated with chemotherapy and/or radiation therapy have a shorter life expectancy, mainly due to an increased risk of death from second cancers. Chemotherapy and radiation therapy have also both been associated with an increased risk of heart and vascular disease.
Balancing the risks and benefits of chemotherapy is an important issue for people with testicular cancer. However, metastatic testicular cancer (see further below) can generally only be cured with chemotherapy. So, for those with metastatic testicular cancer, the benefits of chemotherapy generally greatly outweigh the risks. For people with stage I testicular cancer, the risks of chemotherapy may outweigh the benefits because overall survival rates for testicular cancer are very high regardless of which treatment is given. Talk with your health care team about the potential short-term and long-term side effects of chemotherapy for testicular cancer.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications.
It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation therapy given from a machine outside the body.
For testicular cancer, the radiation therapy is generally directed at lymph nodes in the abdomen for stage I or stage II pure seminoma. Sometimes, the radiation therapy is directed at the lymph nodes on the same side of the pelvis as the testicle where the cancer started.
Radiation therapy for stage I seminoma is now used less often. Surveillance or, less commonly, chemotherapy with carboplatin (see above, under Chemotherapy) is usually used instead of radiation therapy as the preferred treatment of stage I seminoma at many treatment centers because of the risk that radiation therapy may cause other cancers and heart disease. However, radiation therapy remains an option for stage I, IIA, and IIB pure seminoma. It is also sometimes used to treat brain metastases from either seminoma or non-seminoma, but testicular cancer rarely spreads to the brain.
Side effects from radiation therapy
Side effects from radiation therapy may include fatigue, mild skin reactions, upset stomach, loose bowel movements, and peptic ulcers. Medications may be helpful to prevent or reduce nausea and vomiting during radiation therapy. Most side effects go away soon after treatment is finished. Radiation therapy may cause problems with sperm production, but this is less common now with newer radiation techniques that can help preserve fertility.
Radiation therapy increases the risk of secondary cancers many years after treatment and may increase the risk of heart problems and gastrointestinal disease. Recent data indicates that people with testicular cancer who are treated with chemotherapy and/or radiation therapy have a shorter life expectancy, mainly due to an increased risk of death from second cancers and from diseases of the digestive system. Talk with your doctor about your risk of long-term side effects before starting radiation therapy.
Learn more about the basics of radiation therapy.
Return to top
Treatment by stage of testicular cancer
Different treatments may be recommended for each stage of testicular cancer. The general options by stage are described below. For more detailed descriptions, see “How testicular cancer cancer is treated,” above. Clinical trials may also be a treatment option for each stage. The treatment choices for testicular cancer depend on whether the cancer is a seminoma or non-seminoma (see Introduction) and the stage of the cancer (see Stages). After a physical examination, staging tests, and the removal of the cancerous testicle, you and your doctor will discuss your options and decide on your personal treatment plan.
Clinical stage I non-seminoma testicular cancer
About 75% of patients with clinical stage I non-seminoma are cured when the testicle with cancer is removed. But about 25% of patients will have small areas of metastatic cancer that cannot be seen with CT scans when diagnosed. Over time, these areas can grow unless additional treatment is given after orchiectomy. Most recurrences of stage I non-seminoma occur within 9 months after diagnosis and occur in the retroperitoneum. People with clinical stage I disease have the following options after surgery:
-
Surveillance. This option involves CT scans of the abdomen and pelvis every 3 to 6 months for the first year, every 4 to 12 months in the second year, and every 6 to 12 months in the third to fifth year. Physical examinations and tumor marker tests to measure beta-hCG and AFP are done every 1 to 2 months for the first 12 months, every 2 to 3 months in the second year, every 3 to 4 months in the third and fourth years, every 6 months in the fifth year, and then once a year. A chest x-ray is usually needed at every other visit. If the cancer recurs, 3 cycles of chemotherapy successfully treats the cancer for more than 95% of patients. RPLND may be used to treat recurrent cancer if it is limited to the retroperitoneal lymph nodes.
-
RPLND. As described above, this is surgery to remove the retroperitoneal lymph nodes in the back of the abdomen. After RPLND, the risk of recurrence is about 10% on average if no cancer is found in those lymph nodes. Most recurrences after RPLND occur in the lungs or the lymph nodes in the chest, and they almost always occur within 2 years after the RPLND.
-
Chemotherapy. This option involves receiving chemotherapy shortly after the testicle has been removed surgically, called adjuvant chemotherapy. The most commonly used approach has been to give 1 cycle of BEP chemotherapy that lasts 3 weeks. Sometimes, 2 cycles of BEP chemotherapy may be used, but 1 cycle is more common. The advantage of this approach is that it lowers the recurrence rate from 25% to less than 3%. The main disadvantage is that 75% of patients do not need chemotherapy because they have already been cured with the surgical removal of the testicle. Therefore, some doctors do not recommend chemotherapy for clinical stage I non-seminoma, while others may recommend using adjuvant chemotherapy only for those who have a higher risk of recurrence, so that fewer people receive unnecessary treatment.
Clinical stage I seminoma testicular cancer
More than 80% of people with clinical stage I seminoma are cured with orchiectomy alone, while the remaining 15% to 20% will have a recurrence if they are given no additional treatment. Most recurrences occur within 12 months after diagnosis, and the location of the recurrence is typically in the retroperitoneum. Recurrences of stage I seminoma can almost always be cured with radiation therapy, although a few patients will need chemotherapy.
-
Surveillance. Surveillance is the standard method of managing stage I seminoma. Using a surveillance program, the risk of death from stage I seminoma is less than 1%. Unlike surveillance for non-seminoma, someone receiving surveillance for seminoma does not need to visit the doctor as often. While this can vary, a common schedule includes doctor visits every 3 to 6 months for the first 2 years, every 6 to 12 months in the third year, and then yearly until at least 5 years after the original diagnosis. A physical exam should be done at each visit, and some doctors check serum beta-hCG and AFP, although these are not mandatory because they rarely find recurrences that are not seen on CT scans. A CT scan of the abdomen and pelvis should be done every 6 months for the first 2 years, every 6 to 12 months the third year, and then every 12 to 24 months until the patient is 5 years out from orchiectomy. Sometimes chest x-rays are also obtained, but they rarely make a difference because it is uncommon to have the cancer spread to the lungs without also spreading to the abdomen, where it is seen on CT scans.
-
Adjuvant radiation therapy. This is radiation therapy given after surgery. Seminoma is different from non-seminoma, and early-stage seminoma can be effectively treated with radiation therapy. The chance of recurrence can be decreased to less than 5% with 10 to 15 treatments of radiation therapy to the retroperitoneum. Additional radiation therapy to the pelvis does not reduce the overall risk of recurrence, but it does reduce the risk of a recurrence in the pelvis. Some doctors prefer to treat only the retroperitoneum. Others prefer to include the pelvis to prevent recurrences in that area, which means that follow-up with imaging tests of the pelvis is not needed to watch for a recurrence.
The disadvantage of radiation therapy for clinical stage I seminoma is that more than 80% of patients receive treatment that they do not need because they were cured with the orchiectomy. This is a concern because radiation therapy increases the risk of developing other types of cancer, as well as digestive and heart and vascular disease.
-
Adjuvant chemotherapy. This is chemotherapy after surgery. Chemotherapy for stage I seminoma is a newer and more controversial treatment option than surveillance or radiation therapy. Using carboplatin, studies have shown that the risk of recurrence after orchiectomy can be reduced from 18% to about 2% with 2 doses of carboplatin and to about 5% to 6% with 1 dose of carboplatin. Because the use of carboplatin is a newer approach, there is less information on the long-term effects of treatment, and this treatment is controversial. Many experts believe that more information is needed before recommending this treatment approach, while many other experts have accepted carboplatin as a new treatment option for stage I seminoma. Currently, it is listed as a standard treatment option in most testicular cancer treatment guidelines. The hope is that carboplatin will cause fewer problems than radiation therapy, but it won’t be known whether this is the case until the health of those who have received carboplatin has been monitored for a longer period of time. Some problems from cancer treatments do not appear until 10 to 20 years later.
Metastatic testicular cancer
If cancer has spread to another location in the body, it is called metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan. However, testicular cancer is fast-growing, so it is important to start treatment right away. If you want to get a second opinion, talk with the doctor within 1 or 2 weeks after diagnosis.
Your treatment plan is based on many individual factors, including the stage of the cancer (that is, where the cancer has spread) and how high the serum tumor markers are, such as AFP, beta-hCG, and lactate dehydrogenase (LDH). Initial treatment of metastatic testicular cancer is usually chemotherapy. Palliative care will also be important to help relieve symptoms and side effects.
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Clinical stage II non-seminoma testicular cancer
Surgery to remove the testicle is done first, followed by additional treatment. The choice of treatment after orchiectomy depends on a patient’s serum tumor marker levels and the size of retroperitoneal lymph nodes. The treatment options available for people with clinical stage II non-seminoma after surgery are described below. You are encouraged to consider sperm banking for fertility preservation before these treatments begin due to the risk of infertility.
-
Chemotherapy. Chemotherapy is a standard option for anyone with stage II testicular cancer. A combination of drugs is usually given after surgery to remove the testicle. Chemotherapy is the most common treatment for stage IIB and IIC disease and for people with stage IIA disease whose serum tumor markers remain elevated after orchiectomy. For people with stage IIA disease and normal serum tumor markers, chemotherapy or RPLND may be recommended.
-
RPLND. As described above, this is surgery to remove the retroperitoneal lymph nodes in the back of the abdomen. This is a standard treatment option after orchiectomy when the serum tumor marker levels have returned to normal, none of the lymph nodes are larger than 2 cm, and there are no more than 5 enlarged lymph nodes. Chemotherapy may be recommended after RPLND if a large amount of cancer is found in the removed lymph nodes.
Clinical stage II seminoma testicular cancer
Surgery to remove the testicle and lymph nodes with cancer is done first, followed by additional treatment, usually chemotherapy. The main factor in the treatment decision after surgery for a stage II seminoma is the size of the retroperitoneal lymph nodes. You are encouraged to consider sperm banking for fertility preservation before the following treatments begin due to the risk of infertility.
-
Chemotherapy. Chemotherapy with a combination of drugs is given after surgery to remove the testicle. Chemotherapy is a standard treatment option for all stage II seminoma (IIA, IIB, and IIC) and is preferred for stage IIB and stage IIC because it is more likely to get rid of the cancer.
-
Radiation therapy. When lymph nodes are less than 3 cm (stage IIA and early stage IIB), surgery may be followed by radiation therapy to the lymph nodes in the abdomen and pelvis. Sometimes, chemotherapy may be used instead of radiation therapy. Experts disagree about whether radiation therapy or chemotherapy is the preferred option for patients with stage IIA and early stage IIB. Both approaches cure 90% or more of patients with these stages of disease. One advantage of radiation therapy is that it does not increase the risk of developing serious infections, while chemotherapy does. Both chemotherapy and radiation therapy are associated with an increased risk of second cancers and certain other health problems in the future.
Stage III non-seminoma testicular cancer
The following treatment options are available for people with stage III non-seminoma. You are encouraged to consider sperm banking for fertility preservation before treatment begins due to the risk of infertility.
-
Chemotherapy. Chemotherapy is used to treat non-seminoma that has spread beyond the testicles. The most common regimen given is BEP, which is a combination of bleomycin, etoposide, and cisplatin (see "Chemotherapy," above). The treatments are given as 3-week cycles and patients receive either 3 or 4 cycles of chemotherapy for a total treatment period of 9 to 12 weeks. Each drug is given by IV. Cisplatin and etoposide are given each day on the first 5 days. IV fluid is given before and after the cisplatin to reduce the risk of damaging the kidneys. The treatment takes about 6 hours on these days. Bleomycin is given once each week, typically on the first, eighth, and 15th day of the 21-day cycles. The treatment takes about 30 minutes on the days when only bleomycin is given. For patients for whom bleomycin is considered too risky due to age or other factors, 4 cycles of EP chemotherapy can be used for good-risk disease and 4 cycles of VIP chemotherapy can be given for intermediate-risk or poor-risk disease. Both EP and VIP regimens involve giving all of the medications on the first 5 days of a 3-week treatment cycle. VIP chemotherapy is often given in the hospital during a 5-day hospital stay because the treatment lasts for many hours each day.
An important part of the treatment is surgery to remove any remaining masses after chemotherapy ends. The likelihood of chemotherapy successfully treating this cancer depends on the risk group category (see Stages). More than half of metastatic non-seminoma testicular cancers are classified as good risk, and more than 90% of these will be successfully treated with 3 cycles of BEP chemotherapy or 4 cycles of EP chemotherapy.
About 25% of metastatic non-seminomas are intermediate risk, and 80% of these are successfully treated with 4 cycles of BEP plus surgery to remove any remaining masses. About 15% of metastatic non-seminomas are poor risk, and about 50% to 70% of these are cured with 4 cycles of BEP plus surgery to remove any remaining masses. For patients with intermediate risk or poor risk who cannot have bleomycin due to side effects, 4 cycles of VIP chemotherapy has been shown to work just as well as 4 cycles of BEP.
-
Surgery after chemotherapy. After chemotherapy is finished, x-rays and CT scans are done again to see if there are any remaining masses. If there are masses, they are removed with surgery if possible. The chance of the surgery curing the cancer is higher if serum tumor marker levels are normal after chemotherapy. This surgery is difficult and requires an experienced surgeon who regularly performs such operations. Very rarely, if the mass is pressing on the kidney or major blood vessels in the retroperitoneum, the kidney and/or a portion of the blood vessels may need to be removed. Often in this situation the nerves that are responsible for ejaculation cannot be saved.
During surgery, there is about a 35% to 50% chance that only scar tissue will be found, a 35% to 50% chance there will be a teratoma, and a 10% to 15% chance of some other type of germ cell tumor, such as embryonal carcinoma, seminoma, yolk sac tumor, or choriocarcinoma. If only scar tissue and/or a teratoma is found, then no additional treatment is needed. If cancer is found, 2 more cycles of chemotherapy may be given. The chemotherapy regimen used is typically either EP, TIP, VeIP, or VIP.
- Clinical trials. Patients with poor-risk testicular cancer are also encouraged to consider clinical trials as a treatment option.
Stage III seminoma testicular cancer
The following treatment options are available to treat stage III seminoma. You should consider sperm banking for fertility preservation before treatment begins because of the risk of infertility.
-
Chemotherapy. Chemotherapy for metastatic seminoma is the same as for metastatic non-seminoma (see above). About 90% of metastatic seminomas are good risk and are successfully treated with 3 cycles of BEP or 4 cycles of EP. Around 10% of metastatic seminomas are intermediate risk and are generally treated with 4 cycles of BEP or VIP, if bleomycin is considered too risky due the the individual patient's characteristics.
-
Surgery after chemotherapy/radiation therapy. It is quite common for a mass to be found on imaging tests after chemotherapy or radiation therapy is finished. There is less than a 10% chance that this mass contains cancer and almost no chance that it contains a teratoma. The main treatment options are active surveillance or surgery. Such surgery is often very difficult due to a “scar-like” reaction that makes the mass difficult to remove. This is unique to seminoma. Many oncologists recommend surveillance of remaining masses in people with seminomas. Because larger masses are more likely to be cancerous, some doctors recommend surveillance when a mass is smaller than 3 cm and surgery when a mass is 3 cm or larger.
A specific type of positron emission tomography (PET) scan called an FDG PET scan may be used to learn more about the mass. After the PET scan is done, the surgeon will operate only if the scan showed signs of cancer in the remaining mass. The main benefit of a PET scan is to avoid surgery to remove masses that are not cancerous. But recent studies have suggested that PET scan results in these situations may not be accurate. A PET scan may find masses that look like they have cancer, but these masses do not actually contain cancer once they are removed and tested.
If surgery is recommended but the surgeon determines that the mass cannot be removed, a biopsy is often done to try to find out whether the mass is cancerous. If cancer (seminoma) is found, then additional chemotherapy is given. This is called "second-line chemotherapy." If active surveillance is recommended and the mass grows, second-line chemotherapy is the preferred treatment. Surgery can be considered if the mass remains after the chemotherapy.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
Regular follow-up examinations to check for signs that the cancer may be returning are extremely important. If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence). Testicular cancer does not often return as a local recurrence because the entire testicle is removed. Increasing beta-hCG or AFP levels may be a sign that the cancer has returned and more treatment is needed. People who have had a testicular cancer recurrence are encouraged to see a doctor who is an expert in treating recurrent testicular cancer before choosing a treatment approach.
If testicular cancer comes back, a new cycle of testing will begin again to learn as much as possible about the recurrence. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, chemotherapy, and radiation therapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent testicular cancer. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
For recurrent testicular cancer, treatment usually includes chemotherapy and surgery. If the cancer was stage I and returns during active surveillance, then the most common treatment is chemotherapy with 3 or 4 cycles of BEP or 4 cycles of EP, depending on the stage of the cancer. If the cancer is only in the retroperitoneal lymph nodes and is a pure seminoma, then radiation therapy or chemotherapy are both treatment options . If the cancer is only in the retroperitoneal lymph nodes, the serum tumor markers are normal, and the cancer is a non-seminoma, then RPLND or chemotherapy may be recommended. If serum tumor markers are elevated, chemotherapy is generally preferred.
The standard treatment for recurrent testicular cancer that has previously been treated with chemotherapy is either 4 cycles of standard-dose chemotherapy or 2 to 3 cycles of high-dose chemotherapy. The standard-dose chemotherapy regimens include VeIP and TIP. High-dose chemotherapy usually includes carboplatin, etoposide, and sometimes other drugs. It is not known if high-dose chemotherapy works better than standard-dose chemotherapy. If chemotherapy is given, any remaining masses are treated the same way that they are after initial chemotherapy (see above). Third-line chemotherapy options may include oxaliplatin plus gemcitabine, and sometimes paclitaxel is given in addition to those 2 medications.
When the cancer has certain mutations, immunotherapy with pembrolizumab (Keytruda) may also be a treatment option. Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells. Learn more about the basics of immunotherapy.
A recurrence more than 2 years after treatment should be removed with surgery, if possible. Chemotherapy may or may not be recommended after surgery.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with a cancer recurrence.
Return to top
If treatment does not work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.