ON THIS PAGE: You will learn about the different treatments doctors use for people with thyroid cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for thyroid cancer. “Standard of care” means the best treatments known. Information in this section is based on medical standards of care for thyroid cancer in the United States. Treatment options can vary from one place to another.
When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials offer additional options to consider. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How thyroid cancer is treated
In many cases, a team of doctors who specialize in cancer, called oncologists, works together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. For thyroid cancer, this team may include a surgeon, medical oncologist, radiation oncologist, radiologist, nuclear medicine physician, and endocrinologist. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, speech therapists, physical therapists, occupational therapists, and others. Learn more about the clinicians who provide cancer care.
Thyroid cancer is commonly treated by one or a combination of treatments. The common types of treatments used for thyroid cancer are listed below, followed by an outline of common cancer treatments given by stage of disease (see Stages).
Treatment options and recommendations depend on several factors, including the type and stage of thyroid cancer, possible side effects, and the patient's preferences and overall health. Take time to learn about your treatment options and be sure to ask questions about things that are unclear. Talk with your health care team about the goals of each treatment and what you can expect while receiving the treatment. These types of conversations are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is important for thyroid cancer because there are different treatment options.
Cancer treatment is often selected based on guidelines that have been recommended by panels of expert physicians. Although most thyroid cancer is curable, there can be different opinions in how to treat thyroid cancer, particularly regarding which combination of treatments to use and the timing of when treatments are done. Patients are encouraged to seek a second opinion before starting treatment because they should be comfortable with the treatment plan they choose and should ask about clinical trials.
Learn more about making treatment decisions.
READ MORE BELOW:
Surgery
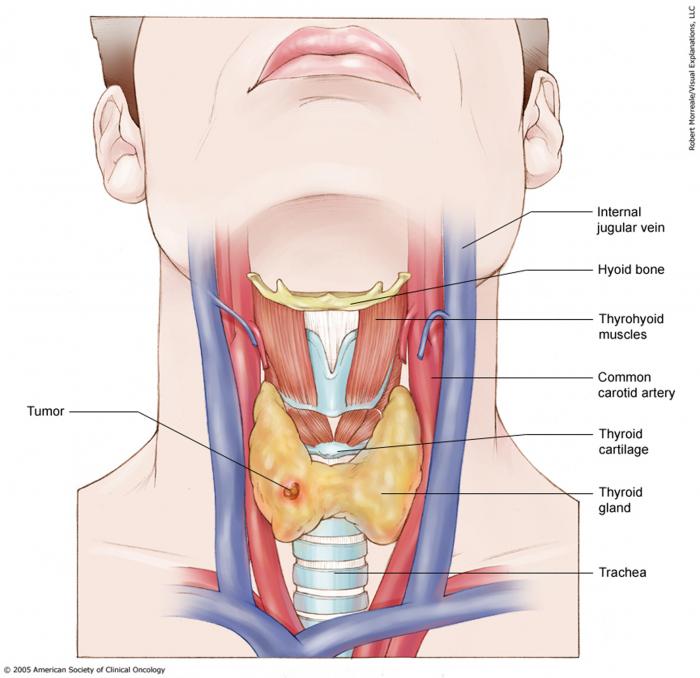
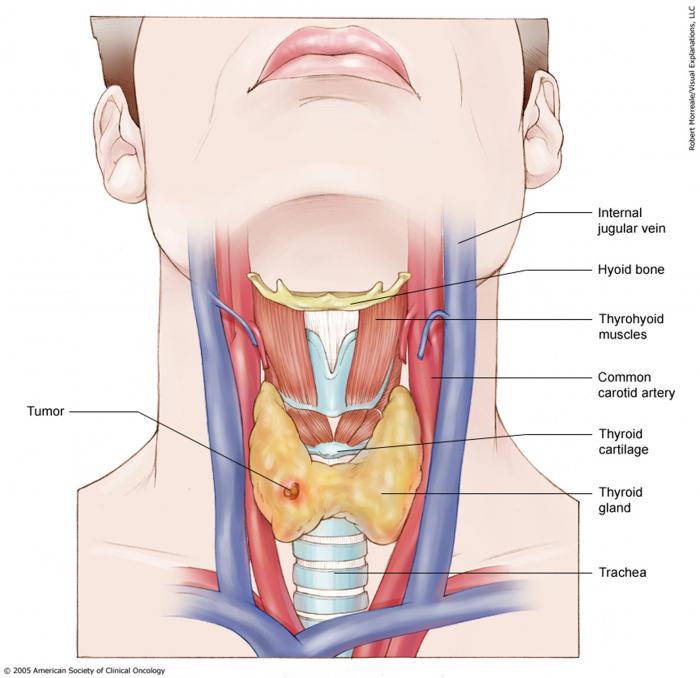
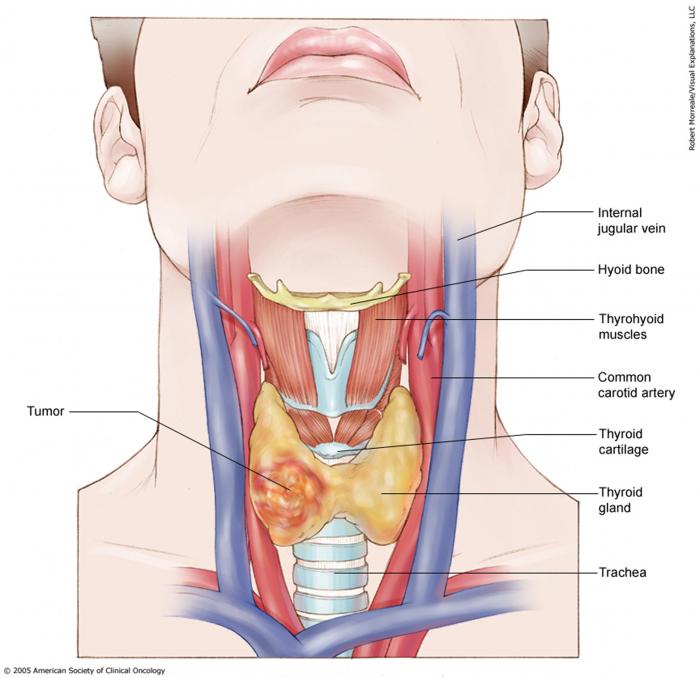
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation, called a margin. Surgery may also be called a resection. It is the main treatment for most people with thyroid cancer. A surgical oncologist is a doctor who specializes in treating cancer using surgery. Depending on the size of the thyroid nodule, common surgical options include:
-
Lobectomy. This surgery removes the lobe of the thyroid gland with the cancerous nodule.
-
Near-total thyroidectomy. Also called subtotal thyroidectomy, this is surgery to removes most of the thyroid gland. A small amount of thyroid tissue remains.
-
Total thyroidectomy. This surgery removes the entire thyroid gland.
There are different surgical techniques that can be used for a thyroidectomy:
-
Standard thyroidectomy. During a standard thyroidectomy, a surgeon makes a small incision (or cut) near the base or middle of the neck. This gives the surgeon direct access to the patient’s thyroid gland for the operation. At some cancer centers, newer surgical techniques are being offered to reduce or avoid neck scarring.
-
Endoscopic thyroidectomy. During an endoscopic thyroidectomy, the surgeon makes a single small incision. The surgery is similar to a standard thyroidectomy except that a scope and video monitor are used to guide the procedure rather than surgical loupe magnification, which is special eyewear.
-
Robotic thyroidectomy. The surgeon makes an incision elsewhere, such as in an armpit, the hairline of the neck, mouth or the chest, and then uses a robotic tool to perform the thyroidectomy. Robotic thyroidectomy is not a recommended surgery for thyroid cancer.
Not all surgical options are recommended for all patients. Talk with your doctor about the best approach to treat you.
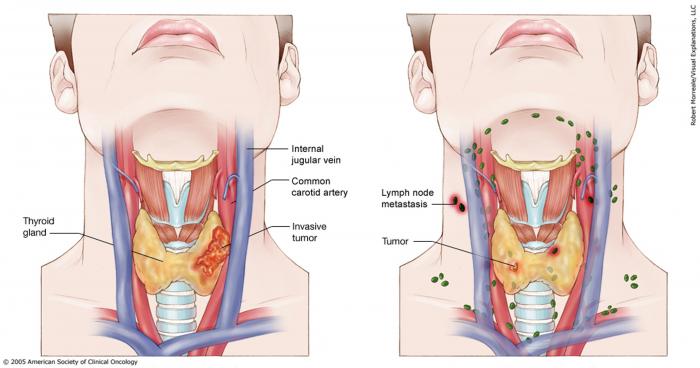
If there is evidence or risk of spread of cancer to the lymph nodes in the neck, the surgeon may also perform a neck dissection. This is surgery to remove the lymph nodes in the neck. Neck dissection is also called lymphadenectomy.
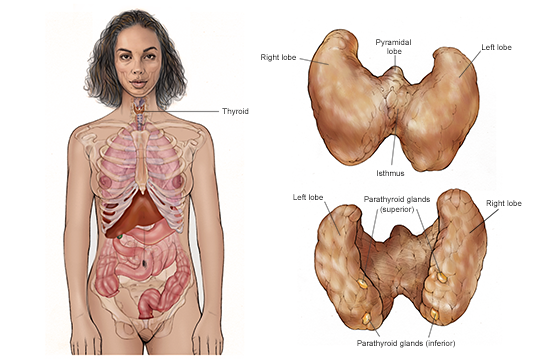
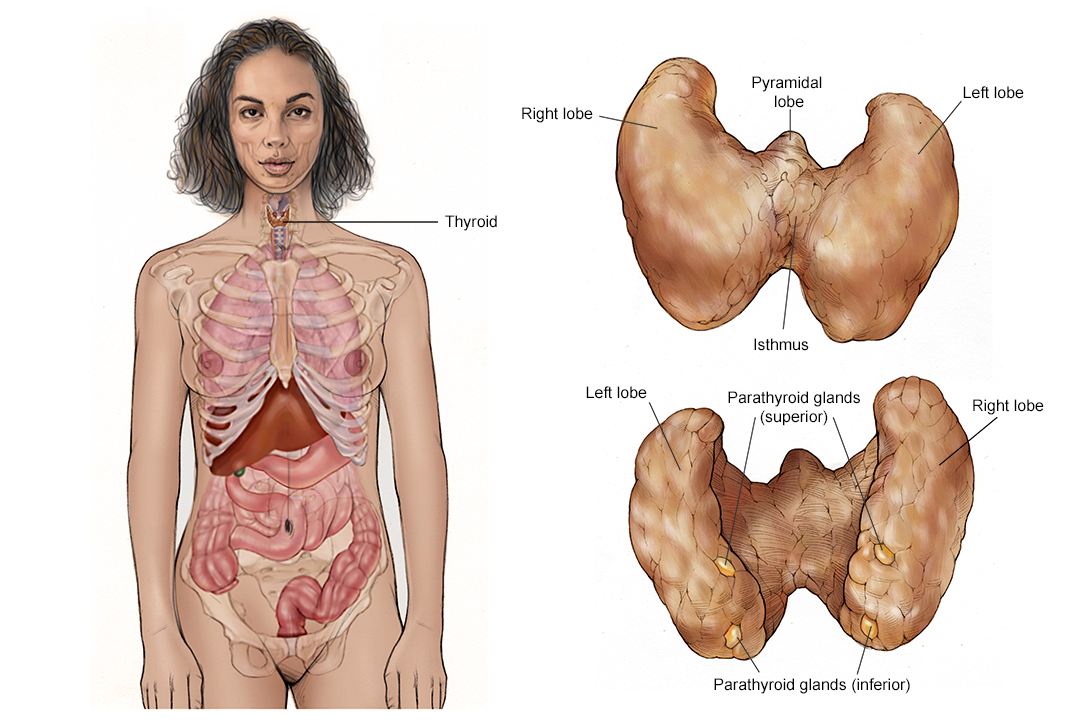
In general, complications of thyroid surgery may include damage to the nearby parathyroid glands, which help regulate blood calcium levels, excessive bleeding, or wound infections. If the nerves to the larynx are damaged during surgery, this may cause temporary or permanent hoarseness or a “breathy” voice.
Without the thyroid gland, the body stops producing thyroid hormone, which is essential to the body’s function. Hormone replacement (see below), usually given by a daily pill, is the best solution. The patient may also have to take vitamin D and calcium supplements if the parathyroid gland's function is reduced after surgery.
If a tumor cannot be removed using surgery, it is called unresectable or inoperable. The doctor will then recommend other treatment options.
Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have and what you can expect during your recovery. Learn more about the basics of cancer surgery.
Return to top
Hormone treatment
Patients who are treated with surgery usually require thyroid hormone therapy. In addition to replacing the hormone that is needed by the body, the thyroid hormone medication may slow down the growth of any remaining differentiated cancer cells.
Thyroid hormone replacement is levothyroxine (Levothroid, Levoxyl, Synthroid, Tirosint, Unithroid, and other brand names.) Levothyroxine typically comes as a pill that should be taken daily, at the same time each day before meals, so that the body receives a consistent supply. Thyroid hormone replacement is usually prescribed by an endocrinologist, which is a doctor specializing in treating problems with hormones, glands, and the endocrine system.
Also, be sure to talk with your doctor about all other medications you take, including dietary supplements such as iron or calcium, to avoid interactions with your thyroid hormone replacement. Read more about tips to take your medication correctly.
Thyroid pills may have a few side effects. Occasionally, some patients develop a rash or lose some hair during the first months of treatment.
Hyperthyroidism is a condition in which there is too much thyroid hormone. It may cause weight loss, chest pain, rapid heart rate, irregular heartbeat, cramps, diarrhea, a feeling of being hot, sweats, and bone loss or osteoporosis.
Hypothyroidism is a condition in where there is too little thyroid hormone. It may cause fatigue, weight gain, dry skin and hair, and a feeling of being cold.
The required amount, called a dose, of thyroid hormone is different for every patient and tumor type, and it can change as a person ages or when weight changes. The doctor will monitor your thyroid hormone levels through regular blood tests. Talk with your doctor about what signs to watch for that may mean it is time to adjust your dose of thyroid hormone supplement.
Learn more about the basics of hormone therapy.
Return to top
Radioactive iodine therapy
The thyroid absorbs almost all iodine that enters a body. Therefore, a type of radiation therapy called radioactive iodine (also called I-131, radioiodine, or RAI) can find and destroy thyroid cells not removed by surgery and those that have spread beyond the thyroid. Doctors who prescribe radioactive iodine therapy are usually endocrinologists or nuclear medicine specialists.
Radioactive iodine treatment is an option for some people with papillary, follicular, and Hurthle cell thyroid cancer. Radioactive iodine is used to treat people with a differentiated thyroid cancer that have spread to lymph nodes or to distant sites. A small test dose may be given before full treatment to be sure that the tumor cells will absorb the I-131. People with medullary thyroid cancer (MTC) or anaplastic thyroid cancer should not be treated with I-131.
I-131 therapy is given in either liquid or pill form. People who receive I-131 to destroy cancer cells may be hospitalized for 2 to 3 days, depending on several factors, including the dose given. Patients are encouraged to drink fluids to help the I-131 pass quickly through the body. Within a few days, most of the radiation is gone. Talk with your doctor about ways to limit radiation exposure to other people, including children, who may be around you during this treatment and the days following it.
In preparation for I-131 therapy after surgery, patients are usually asked to follow a low-iodine diet for 2 to 3 weeks beforehand. In addition to the low-iodine diet, patients will be asked to either stop taking thyroid hormone replacement pills temporarily or to receive injections of recombinant thyroid-stimulating hormone (Thyrogen) while taking the hormone replacement. If the hormone therapy is stopped during the preparation period, the patient will likely experience the side effects of hypothyroidism (see above, under Hormone Therapy).
It is important to discuss the possible short-term and long-term effects of I-131 therapy with your doctor. On the first day of treatment, patients may experience nausea and vomiting. In certain circumstances, pain and swelling can occur in the areas where the radioactive iodine is collected. Because iodine is concentrated in salivary gland tissue, patients may experience swelling of the salivary glands. This may result in dry mouth, sometimes called xerostomia.
Large or cumulative doses of radioactive iodine may cause infertility, which is the physical inability to have a child, especially in men. Avoiding pregnancy is recommended for at least 1 year after I-131 treatment. There is a risk of secondary cancer with the use of I-131 (see Follow-up Care). Occasionally, patients may require repeated treatments over time. However, there is a maximum total dose of radioactive iodine allowed over time, and once reached, this may prevent further use of this treatment.
Return to top
External-beam radiation therapy
External-beam radiation is another type of radiation therapy in which high-energy x-rays are given from a machine outside the body to destroy cancer cells. A doctor who specializes in external-beam radiation therapy is called a radiation oncologist. An external-beam radiation therapy regimen (schedule) usually consists of a specific number of treatments given over a set period of time. When used to treat thyroid cancer, radiation therapy is usually given as outpatient therapy, either in a hospital or clinic, 5 days a week for about 5 to 6 weeks.
For thyroid cancer, external-beam radiation therapy is used only in certain circumstances, typically when later-stage thyroid cancer has spread to critical areas of the neck such as the trachea, voice box, or esophagus. Radiation therapy is usually given after surgery, and treatment is concentrated on a specific area, only affecting cancer cells at that site. Radiation therapy is usually not used to manage thyroid cancer in younger patients.
Side effects depend on the treatment dosage and area and may include redness of the skin, odynophagia (painful swallowing), cough, occasional hoarseness, nausea, and fatigue. Most side effects go away soon after treatment is finished.
Learn more about the basics of external-beam radiation therapy.
Return to top
Therapies using medication
The treatment plan my include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication.
When used, medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications to take at home, be sure to ask your health care team how to safely store and handle them.
The types of medications used to treat thyroid cancer include:
-
Chemotherapy
-
Targeted therapy
Each of these types of therapies is discussed below in more detail. A person may receive only 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or a combination of different drugs given at the same time.
The side effects of chemotherapy depend on the individual and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away after treatment is finished. Learn more about the basics of chemotherapy.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to normal cells. Learn more about the basics of targeted therapy.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets in the different types of thyroid cancer and new treatments directed at them.
For papillary and follicular thyroid cancers, the U.S. Food and Drug Administration (FDA) has approved several targeted therapies:
Sorafenib (Nexavar) is approved for later-stage or recurrent differentiated thyroid cancer when I-131 therapy (see above) has not worked.
Lenvatinib (Lenvima, E7080) is approved for later-stage differentiated thyroid cancer when surgery, I-131 treatment, or both have not worked.
Larotrectinib (Vitrakvi) is approved for rare cases of papillary and follicular thyroid cancers that have an NTRK gene fusion mutation.
Entrectinib (Rozlytrek) is approved for thyroid tumors with an NTRK gene fusion mutation.
Selpercantinib (Retevmo) and Pralsetinib (Gavreto) are approved for rare cases of advanced metastatic RET fusion-positive thyroid cancer that requires systemic therapy. They can affect the levels of platelets, certain enzymes, and proteins in the body. These levels need to be monitored every 2 weeks during the first 3 months of treatment and then every month after that.
For MTC, the FDA-approved targeted therapy options include:
Vandetanib (Caprelsa, zd6474) is a type of tyrosine kinase inhibitor that is approved to treat MTC when it cannot be removed surgically, if the disease is worsening, or if the MTC has spread to other parts of the body. Additional blood tests may be needed for people who are taking vandetanib because of possible severe side effects. The blood tests will be used to monitor serum potassium, calcium, magnesium, and thyroid-stimulating hormone (TSH) levels (see Diagnosis) to regularly check the body's reaction to this medication.
Cabozantinib (Cometriq, Cabometyx, XL184) is a type of tyrosine kinase inhibitor that is approved for metastatic MTC. It is also approved to treat differentiated thyroid cancer that has progressed after prior treatment with VEGFR-targeted therapy in people who cannot receive radioactive iodine treatment.
Selpercatinib (see above) is also approved to treat people with advanced or metastatic RET-mutant MTC.
For anaplastic thyroid cancer, there is 1 targeted therapy combination approved by the FDA:
Dabrafenib (Tafinlar) and trametinib (Mekinist) are approved to treat people with anaplastic thyroid cancer with a specific mutation in the BRAF gene. Dabrafenib is a BRAF inhibitor and trametinib is a MEK inhibitor. This combination is now a standard of care for anaplastic thyroid cancer that cannot be removed surgically or has spread to distant areas.
Before any targeted treatment begins, talk with your doctor about possible side effects for each specific medication and how they can be managed. Common side effects of targeted therapies include skin problems, diarrhea, fatigue, blood pressure problems, constipation, nausea, and vomiting.
Return to top
Chemotherapy or targeted therapy as part of your treatment plan
At this time, the use of other systemic chemotherapy and targeted therapy for the treatment of thyroid cancer is determined on an individual basis and is most often given as part of a clinical trial. See the Latest Research section for more information.
Learn more about the basics of preparing for treatment. The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions by using searchable drug databases.
Return to top
Physical, emotional, social, and financial effects of cancer
Thyroid cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative and supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative and supportive care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative and supportive care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments such as chemotherapy, surgery, or radiation therapy, to improve symptoms.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative and supportive care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Return to top
Treatment options by stage
Almost all thyroid cancers are treated with surgery. If the thyroid cancer is only within the tissues of the neck, both in the thyroid gland and in the lymph nodes, surgery will typically be the first treatment. Patients with later-stage disease may be treated with surgery as well, but other treatments may be done first. Clinical trials may be recommended at any stage as a treatment option.
Hormone therapy and radioactive iodine therapy are only given for papillary, follicular, and Hurthle cell thyroid cancers. MTC and anaplastic thyroid cancers are not managed with radioactive iodine thyroid or thyroid hormone therapy.
Stage I: Surgery, hormone therapy, possible radioactive iodine therapy after surgery
Stage II: Surgery, hormone therapy, possible radioactive iodine therapy after surgery
Stage III: Surgery, hormone therapy, possible radioactive iodine therapy or external-beam radiation therapy after surgery
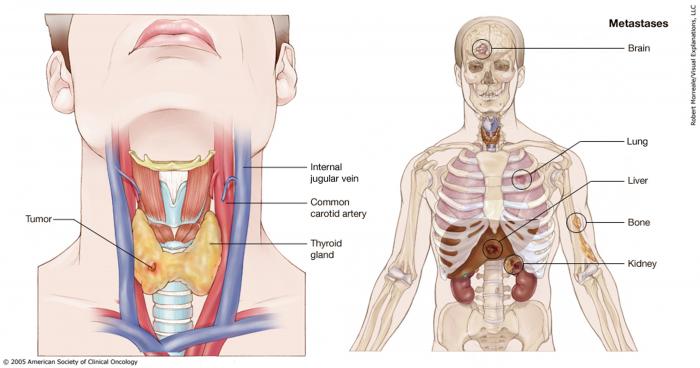
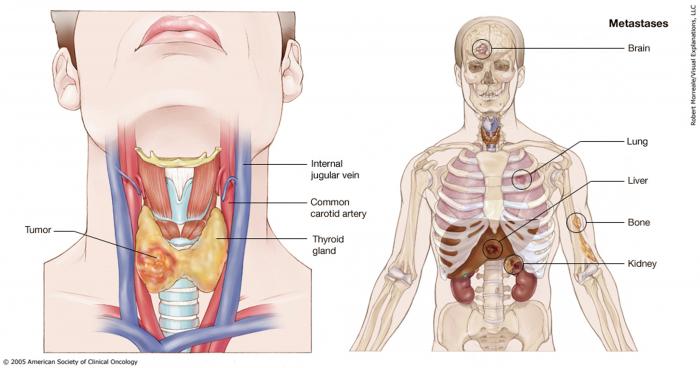
Stage IV: Surgery, hormone therapy, radioactive iodine therapy, external-beam radiation therapy, targeted therapy, and chemotherapy. Radiation therapy may also be used to reduce pain and other problems. See below for more information, for "Metastatic thyroid cancer."
Return to top
Metastatic thyroid cancer
If the cancer has spread beyond the thyroid to other organs, such as the bones or lungs, it is called metastatic or stage IV thyroid cancer. Also, all anaplastic thyroid tumors are classified as stage IV at the time of diagnosis, regardless of tumor size, location, or spread.
If the diagnosis is stage IV thyroid cancer, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
Your treatment plan may include a combination of surgery, hormone therapy, radioactive iodine therapy, external-beam radiation therapy, targeted therapy, and chemotherapy. Clinical trials on new treatment approaches may also be recommended. Palliative and supportive care will also be important to help relieve symptoms and side effects
For most people, a diagnosis of metastatic cancer is very stressful and difficult to bear. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence).
If a recurrence happens, a new cycle of testing will begin to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options.
Often the treatment plan will include the treatments described above, such as surgery, radioactive iodine therapy, targeted therapy, external-beam radiation therapy, hormone therapy, and chemotherapy. However, they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent thyroid cancer. Whichever treatment plan you choose, palliative and supportive care will be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Return to top
If treatment does not work
Recovery from thyroid cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
Planning for your future care and putting your wishes in writing is important, especially at this stage of disease. Then, your health care team and loved ones will know what you want, even if you are unable to make these decisions. Learn more about putting your health care wishes in writing.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life.
You and your family are encouraged to talk with your doctor or a member of your palliative care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.