ON THIS PAGE: You will learn about the different types of treatments doctors use for people with non-small cell lung cancer (NSCLC). Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for NSCLC. “Standard of care” means the best treatments known. When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials are an option. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether the new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How NSCLC is treated
In cancer care, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of talks are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is particularly important for NSCLC because there are different treatment options. Learn more about making treatment decisions.
The common types of treatments used for NSCLC are described below, followed by an outline of the common treatment plans by stage. Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
Surgery
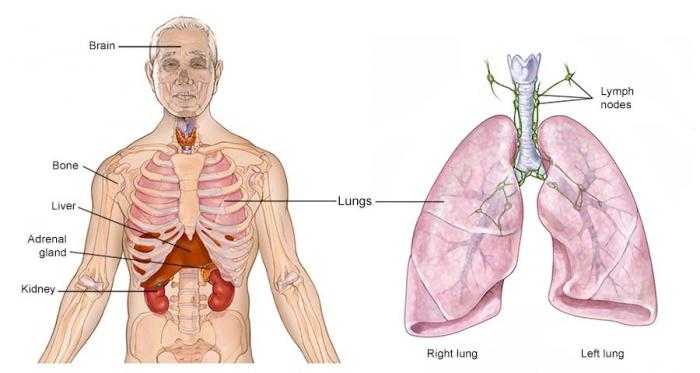
The goal of surgery is to completely remove the lung tumor and the nearby lymph nodes in the chest. The tumor must be removed with a surrounding border or margin of healthy lung tissue. A “negative margin” means that when the pathologist examined the lung or a piece of lung that was removed by the surgeon, no cancer was found in the healthy tissue surrounding the tumor. A surgical oncologist is a doctor who specializes in treating cancer using surgery. A thoracic surgeon is specially trained to perform lung cancer surgery.
The following types of surgery may be used for NSCLC:
-
Lobectomy. The lungs have 5 lobes, 3 in the right lung and 2 in the left lung. A lobectomy is the removal of an entire lobe of the lung. It is currently thought to be the most effective type of surgery, even when the lung tumor is very small. Clinical trials are underway to study if less extensive surgeries have similar outcomes for tumors that are 2 centimeters or smaller.
-
A wedge resection. If the surgeon cannot remove an entire lobe of the lung, the surgeon can remove the tumor, surrounded by a margin of healthy lung.
-
Segmentectomy. This is another way to remove the cancer when an entire lobe of the lung cannot be removed. In a segmentectomy, the surgeon removes the portion of the lung where the cancer developed. Typically, more lung tissue and lymph nodes are removed during a segmentectomy compared to a wedge resection.
-
Pneumonectomy. If the tumor is close to the center of the chest, the surgeon may have to remove the entire lung. A pneumonectomy has more risks than a lobectomy and your doctor will need to consider the health of your heart and lungs before performing this surgery.
The time it takes to recover from lung surgery depends on how much of the lung is removed and the person's health before surgery. Exercise can be an important part of preparing for and recovering from surgery. It can help prevent or relieve side effects and shorten time in the hospital. Ask your doctor what type of exercise is recommended for you. While many patients can safely exercise on their own, some may need to exercise with the guidance of a member of the health care team or to participate in a cancer rehabilitation program before exercising on their own.
Many of these surgeries are now minimally invasive compared to the past. Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have. Learn more about the basics of cancer surgery.
Additional treatments can be given before and after your surgery to help lower the risk of recurrence.
Neoadjuvant therapy, also known as induction therapy, is a therapy given before your surgery. In addition to treating the primary tumor and lowering your risk of recurrence, this type of therapy is also used to help reduce the extent of surgery.
Adjuvant therapy is treatment that is given after surgery. It is intended to get rid of any lung cancer cells that may still be in the body after surgery. This helps lower the risk of recurrence, though there is always some risk that the cancer will come back.
These types of adjuvant therapy used for NSCLC include radiation therapy and systemic therapies, such as chemotherapy, targeted therapy, and immunotherapy. Sometimes adjuvant therapies will combine treatments, such as chemotherapy and immunotherapy. Each therapy is described below.
Return to top
Radiation therapy
Radiation therapy is the use of high energy x-rays or other particles to destroy cancer cells. If you need radiation therapy, you will see a specialist called a radiation oncologist. A radiation oncologist is the doctor who specializes in giving radiation therapy to treat cancer. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. This can vary from just a few days of treatment to several weeks.
Like surgery, radiation therapy cannot be used to treat widespread cancer. Radiation therapy only destroys cancer cells directly in the path of the radiation beam. It also damages the healthy cells in its path. For this reason, it cannot be used to treat large areas of the body. The most common type of radiation is intensity modulated radiation therapy (IMRT). For some people, their tumors require a specialized type of radiation such as stereotactic body radiation therapy (SBRT) or proton therapy. These types of radiation therapy use CT scans or PET scans to plan out exactly where to direct the radiation beam to lower the risk of damaging healthy parts of the body. It is not an option for all patients, but it may be used for early-stage disease and for a small tumor when surgery is not an option.
Some people with stage I NSCLC or people who cannot have surgery may be treated with stereotactic radiation therapy instead of surgery.
Listen to a Cancer.Net Podcast on ASCO’s recommendations for radiation therapy for NSCLC.
Side effects of radiation therapy
People with lung cancer who receive radiation therapy often experience fatigue and loss of appetite. If radiation therapy is given to the neck or center of the chest, side effects can include a sore throat and difficulty swallowing. Patients may also notice skin irritation, similar to sunburn, where the radiation therapy was directed. Most side effects go away soon after treatment is finished.
If the radiation therapy irritates or inflames the lung, patients may develop a cough, fever, or shortness of breath months and sometimes years after the radiation therapy ends. About 15% of patients develop this condition, called radiation pneumonitis. If it is mild, radiation pneumonitis does not need treatment and goes away on its own. If it is severe, a patient may need treatment for radiation pneumonitis with steroid medications, such as prednisone (Rayos).
Radiation therapy may also cause permanent scarring of the lung tissue near where the original tumor was located. The scarring does not usually cause symptoms. However, severe scarring can cause a permanent cough and shortness of breath. For this reason, radiation oncologists carefully plan the treatments using CT scans of the chest to lessen the amount of healthy lung tissue exposed to radiation (see above).
Learn more about the basics of radiation therapy.
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication.
Medications are often given through an intravenous (IV) tube placed into a vein using a needle or in a pill or capsule that is swallowed (orally). If you are given oral medications, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for NSCLC include:
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
Each of these types of therapies are discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. It has been shown to improve both the length and quality of life for people with lung cancer of all stages.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. The type of lung cancer you have, such as adenocarcinoma or squamous cell carcinoma, affects which drugs are recommended for chemotherapy. When adjuvant chemotherapy is given after surgery, it is usually given for a shorter period of time (such as 4 cycles) than for those with stage IV lung cancer.
Common drugs used to treat lung cancer include either 2 or 3 drugs given together or 1 drug given by itself. Some common drugs include:
-
Carboplatin (available as a generic drug)
-
Cisplatin (available as a generic drug)
-
Docetaxel (Taxotere)
-
Etoposide (available as a generic drug)
-
Gemcitabine (Gemzar)
-
Nab-paclitaxel (Abraxane)
-
Paclitaxel (Taxol)
-
Pemetrexed (Alimta)
-
Vinorelbine (Navelbine)
Chemotherapy may also damage healthy cells in the body, including blood cells, skin cells, and nerve cells. The side effects of chemotherapy depend on the person and the dose used, but they can include fatigue, low numbers of blood cells, risk of infection, mouth sores, nausea and vomiting, loss of appetite, diarrhea, numbness and tingling in the hands and feet, and hair loss. Some lung cancer chemotherapy treatments do not cause significant hair loss. Your medical oncologist can often prescribe drugs to help relieve many of these side effects. Nausea and vomiting are also often avoidable. Learn more about preventing nausea and vomiting caused by cancer treatment. In many cases, side effects usually go away after treatment is finished.
Learn more about the basics of chemotherapy.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in the tumor. For some lung cancers, abnormal proteins are found in unusually large amounts in the cancer cells. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments.
Treatment with targeted therapy for NSCLC is changing rapidly due to the pace of scientific research. New targeted therapies are being studied in clinical trials now. Talk with your doctor about additional options that may be available to you.
Targeted therapy for NSCLC includes:
Epidermal growth factor receptor (EGFR) inhibitors. About 10% to 15% of all lung cancers are EGFR-positive. Researchers have found that drugs that block specific EGFR mutations may be effective for stopping or slowing the growth of lung cancer when the cancer cells have that EGFR specific mutation. The following EGFR inhibitors are approved by the FDA:
-
Afatinib (Gilotrif)
-
Dacomitinib (Vizimpro)
-
Erlotinib (Tarceva)
-
Gefitinib (Iressa)
-
Osimertinib (Tagrisso)
Drugs targeting the EGFR exon 20 insertion. Some people have a specific change to the EGFR gene in the exon 20. This is called an EGFR exon 20 insertion. The following drug has been approved to target EGFR exon 20 insertion as a second-line treatment:
Drugs targeting HER2 mutations. Human epidermal growth factor receptor 2 (HER2) mutations help cancer cells grow and spread. HER2 mutations have been found in 1% to 4% of NSCLC cases. One drug is approved to target HER2 mutations in people who have received a prior systemic therapy, when confirmed by an FDA-approved test:
Anaplastic lymphoma kinase (ALK) inhibitors. ALK is a protein that is a part of the cell growth process. When present, this helps cancer cells grow. ALK inhibitors help stop this process. Changes in the ALK gene are found in about 4% of people with NSCLC. The following drugs are currently available to target this genetic change:
-
Alectinib (Alecensa)
-
Brigatinib (Alunbrig)
-
Ceritinib (Zykadia)
-
Crizotinib (Xalkori)
-
Lorlatinib (Lorbrena)
Drugs targeting ROS1 fusion. Rare changes to the ROS1 gene called ROS1 fusion or ROS1 rearrangement can cause problems with cell growth and cell differentiation. Cell differentiation is the process by cells use to change from one type of cell into another. ROS1 fusion is found in 1% to 2% of people with lung cancer. Drugs targeting changes to the ROS1 gene include:
-
Ceritinib (Zykadia)
-
Crizotinib (Xalkori)
-
Entrectinib (Rozlytrek)
Drugs targeting KRAS G12C mutations. The KRAS G12C is one of the most common genetic mutations found in people with NSCLC. About 20 to 25% of people with lung cancer have a KRAS mutation. Two drugs are approved to target KRAS G12C mutations in the second-line setting, after receiving immunotherapy alone or in combination with chemotherapy:
-
Adagrasib (Krazati)
-
Sotorasib (Lumakras)
Drugs targeting NTRK fusion. This type of genetic change is found in a range of cancers and causes cancer cell growth. It is rare in lung cancer (less than 1%). One drug is approved to target NTRK fusion:
-
Entrectinib (Rozlytrek)
-
Larotrectinib (Vitrakvi)
Drugs targeting BRAF V600E mutations. The BRAF gene makes a protein that is involved in cell growth and can cause cancer cells to grow and spread. BRAF mutations have been found in 4% of NSCLC cases. Metastatic NSCLC with BRAF V600E mutations can be targeted with the following drugs:
Drugs targeting MET exon 14 skipping. MET exon 14 skipping is a genetic mutation found in over 3% of NSCLC cases. Drugs approved to treat MET exon 14 skipping include:
-
Capmatinib (Tabrecta)
-
Tepotinib (Tepmetko)
Drugs targeting RET fusion. Up to 2% of all NSCLC cases are RET fusion positive. Drugs approved to target RET fusion positive NSCLC include:
-
Pralsetinib (Gavreto)
-
Selpercatinib (Retevmo)
Anti-angiogenesis therapy. Anti-angiogenesis therapy stops angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumor. The following anti-angiogenic drugs may be options for lung cancer:
-
Bevacizumab (Avastin, Mvasi), in combination with chemotherapy and atezolizumab (Tecentriq), an immunotherapy drug (see below)
-
Ramucirumab (Cyramza), in combination with the chemotherapy drug docetaxel
Immunotherapy (updated 04/2023)
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system's ability to attack cancer cells.
People who receive treatment using immunotherapy for NSCLC may receive only 1 drug, a combination of immunotherapy drugs, or it may be combined with chemotherapy. When advanced NSCLC cannot be treated with a targeted therapy (see above), immunotherapy or immunotherapy plus chemotherapy is often the preferred initial treatment.
There are different ways immunotherapy can use the body's immune system to treat cancer.
Drugs that block the PD-1 pathway. The PD-1 pathway may be very important in the immune system's ability to control cancer growth. Blocking this pathway with PD-1 and PD-L1 antibodies has stopped or slowed the growth of NSCLC for some patients. The following immunotherapy drugs block this pathway and are approved to treat NSCLC:
In certain cases, immunotherapy may be combined with platinum-based chemotherapy, such as cemipilmab-rwlc or durvalumab.
Drugs that block the CTLA-4 pathway. Another immune pathway that may be targeted is the CTLA-4 pathway:
-
Ipilimumab (Yervoy). Ipilimumab is given in combination with nivolumab, which blocks the PD-1 pathway. This combination can also be used with chemotherapy.
-
Tremelimumab (Imjudo). Tremelimumab may be given in combination with durvalumab and chemotherapy. This combination is used to treat metastatic NSCLC without a targeted mutation in the EGFR or ALK genes.
Different types of immunotherapy can cause different side effects but, in general, severe side effects are less common than with chemotherapy. Immune-related side effects are possible with immunotherapy and include skin reactions, flu-like symptoms, diarrhea, shortness of breath from lung inflammation, and weight changes. The risk of immune-related side effects is higher if a PD-1/PD-L1 inhibitor is combined with a CTLA-4 inhibitor. Talk with your doctor about possible side effects for the immunotherapy recommended for you.
Learn more about the basics of immunotherapy and its side effects.
Return to top
Physical, emotional, and social effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
The following treatments may be given to help relieve the symptoms of NSCLC:
-
A tumor in the chest that is bleeding or blocking the lung passages can be shrunk with radiation therapy.
-
During a bronchoscopy (See Diagnosis), lung passages blocked by cancer can be opened to improve breathing.
-
A surgeon or pulmonologist can place a stent to prop open an airway or use a laser to burn away a tumor.
-
Medications are used to treat cancer pain. Most hospitals and cancer centers have pain control specialists who provide pain relief, even for severe cancer pain. Many drugs used to treat cancer pain, especially morphine, can also relieve shortness of breath caused by cancer. Learn more about managing cancer pain.
-
Medications can be used to stop a cough, open closed airways, or reduce bronchial secretions.
-
Prednisone can reduce inflammation caused by lung cancer or radiation therapy and improve breathing. Dexamethasone can be used for pain caused by bone metastases, to reduce inflammation or edema from brain and spinal cord metastases, or be used to improve apetite and increase energy.
-
Extra oxygen from small, portable tanks can help make up for the lung’s reduced ability to extract oxygen from the air.
-
Medications are available to strengthen bones, lessen bone pain, and help prevent future bone metastases.
-
Appetite stimulants and nutritional supplements can improve appetite and reduce weight loss.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Return to top
Treatment by stage of NSCLC
Different treatments may be recommended for each stage of NSCLC. The general options by stage are described below. For more detailed descriptions, see "How NSCLC is treated," above. Your doctor will work with you to develop a specific treatment plan based on your specific diagnosis and needs. Clinical trials may also be a treatment option for each stage.
Stage I and II NSCLC (updated 01/2023)
In general, stage I and stage II NSCLC are treated with surgery. Surgeons cure many people with an operation.
Before or after surgery, a patient may also meet with a medical oncologist. Some people with a large tumor or signs that the tumor has spread to the lymph nodes may benefit from treatments with medication, sometimes called systemic treatments, including chemotherapy, immunotherapy, and/or targeted therapies. Medication may be given before the surgery, called neoadjuvant therapy or induction therapy. Additional treatment may also be given after surgery, called adjuvant therapy, to reduce the chance that the cancer will return. The decision to use neoadjuvant therapy before surgery or adjuvant therapy after surgery is the most appropriate approach is complex. It often requires a multidisciplinary discussion between surgeons, medical oncologists, radiation oncologists, radiologists, pulmonologists, and pathologists. These discussions usually occur at a type of meeting called a tumor board. This discussion will be done after all information from the initial biopsies and imaging are available for review and before a surgery or systemic therapy is started.
Adjuvant chemotherapy with cisplatin is not recommended for patients with stage IA NSCLC that was completely removed with surgery. Patients with stage IB cancers should talk with their doctors about whether chemotherapy is right for them after surgery. For those with stage IB cancer with an activating EGFR mutation, ASCO recommends targeted therapy with adjuvant osimertinib for up to 3 years. Adjuvant cisplatin-based chemotherapy is recommended for patients with stage II NSCLC that has been completely removed with surgery. Patients with stage II NSCLC should talk with their doctor about whether this treatment is right for them. If there is not an activating EGFR mutation, treatment with atezolizumab for up to 1 year may be recommended, particularly if the tumor's PD-L1 expression is high. Recently, the FDA also approved the use of pembrolizumab after surgery in patients with stage IB to stage III NSCLC.
For patients with stage I or II lung cancer who cannot or prefer not to undergo surgery, radiation therapy, such as stereotactic ablative radiotherapy (SABR) or stereotactic body radiotherapy (SBRT), may be offered.
Stage III NSCLC (updated 06/2023)
More than 30,000 people are diagnosed with stage III NSCLC every year, and there is no single best treatment for all of these patients. Treatment options depend on the size and location of the tumor and the lymph nodes that are involved. The options generally include:
-
Radiation therapy
-
Chemotherapy
-
Immunotherapy
-
Targeted therapy
-
Surgery
Chemotherapy and radiation therapy may be given together, which is called concurrent chemoradiotherapy. Or, they may be given one after the other, called sequential chemoradiotherapy.
If the stage III NSCLC cannot be removed with surgery, ASCO recommends concurrent chemoradiotherapy using a platinum-based chemotherapy combination. If concurrent chemoradiotherapy has slowed or stopped the cancer’s growth, immunotherapy with durvalumab for up to 1 year after completion of chemoradiotherapy is recommended. If concurrent chemoradiotherapy is not an option, ASCO recommends sequential chemoradiotherapy instead.
Surgery may be an option for some people with stage III NSCLC if the tumor and lymph nodes can be removed without leaving cancer behind and the side effects and complications from the surgery are expected to be low. If surgery is an option, systemic therapy using chemotherapy, immunotherapy, and/or concurrent chemoradiotherapy will usually be given before the surgery. After surgery, adjuvant platinum-based chemotherapy and/or osimertinib or atezolizumab may be offered, including for people with common EGFR mutations. Recently, the FDA also approved the use of pembrolizumab after surgery in patients with stage IB to stage III NSCLC. Radiation therapy is not generally recommended after surgery, though it may be recommended in some cases where cancer cells are left behind after surgery.
Talk with your health care team about the best treatment options for you.
This information is based on the ASCO guideline, “Management of Stage III NSCLC.” Please note that this link takes you to a different ASCO website.
Metastatic or stage IV NSCLC
If cancer spreads to another part in the body from where it started, doctors call it metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
Patients with stage IV NSCLC typically do not receive surgery or radiation therapy as the main treatment. In some cases, radiation to treat a specific symptom or particularly problematic area may be used.
People with stage IV disease have a very high risk of the cancer spreading or growing in another location. Most patients with this stage of NSCLC receive systemic therapies, such as chemotherapy, targeted therapy, or immunotherapy. Palliative care will also be important to help relieve symptoms and side effects.
Systemic therapy for metastatic or stage IV NSCLC (Updated 07/2023)
The goals of systemic therapies are to shrink the cancer, relieve discomfort caused by the cancer, prevent the cancer from spreading further, and lengthen a patient’s life. These treatments can occasionally make metastatic lung cancer disappear. However, doctors know from experience that the cancer will usually return.
Systemic therapy and palliative care have been proven to improve both length and quality of life for patients with stage IV NSCLC. If the cancer worsens or causes too many severe side effects, the treatment may be stopped. Patients would continue to receive palliative care and may be offered treatment in a clinical trial.
The first drug or combination of drugs a patient takes is called “first-line” treatment, which may be followed by “second-line” and “third-line” treatment. No specific treatment or combination of treatments works for every patient. If the first-line treatment causes too many or dangerous side effects, does not appear to be working, or stops working, the doctor may recommend a change in treatment. ASCO’s recommendations for systemic therapies for NSCLC are included below. All patients should also receive palliative care.
First-line treatment. Two key variables to consider when determining treatment are PD-L1 score and whether there are alterations in the DNA that can be targeted with certain medications.
-
No changes in the EGFR, ALK, ROS1, BRAF, MET, RET, NTRK genes
-
Non-squamous cell carcinoma with PD-L1 50% or higher:
-
Pembrolizumab alone
-
Atezolizumab alone
-
Combination of pembrolizumab, carboplatin, and pemetrexed
-
Combination of atezolizumab, carboplatin, paclitaxel, and bevacizumab
-
Combination of atezolizumab, carboplatin, and nab-paclitaxel
-
Nivolumab and ipilimumab plus platinum-based chemotherapy
-
Cemiplimab alone
-
Nivolumab plus ipilimumab
-
Non-squamous cell carcinoma and PD-L1 1% to 49%:
-
Nivolumab and ipilimumab plus platinum-based chemotherapy
-
Combination of nivolumab and ipilimumab
-
Pembrolizumab combined with carboplatin and pemetrexed
-
Combination of atezolizumab, carboplatin, paclitaxel, and bevacizumab
-
Combination of atezolizumab, carboplatin, and nab-paclitaxel.
-
Cemiplimab plus chemotherapy
-
Durvalumab and tremelimumab plus platinum-based chemotherapy
-
For people who cannot receive immunotherapy, a combination of 2 chemotherapy drugs is recommended.
-
Pembrolizumab alone may be recommended for people who cannot receive a combination of pembrolizumab with a platinum chemotherapy.
-
Non-squamous cell carcinoma and PD-L1 less than 1%:
-
Nivolumab and ipilimumab plus platinum-based chemotherapy
-
Nivolumab and ipilimumab
-
Pembrolizumab combined with carboplatin and pemetrexed
-
Combination of atezolizumab, carboplatin, paclitaxel, and bevacizumab
-
Combination of atezolizumab, carboplatin, and nab-paclitaxel
-
Cemiplimab plus chemotherapy
-
Durvalumab and tremelimumab plus platinum-based chemotherapy
-
For people who cannot receive immunotherapy, a combination of 2 chemotherapy drugs is recommended
-
Squamous cell carcinoma and PD-L1 50% or higher:
-
Atezolizumab alone
-
Cemiplimab alone
-
Pembrolizumab alone
-
Combination of nivolumab and ipilimumab
-
Nivolumab and ipilimumab plus platinum-based chemotherapy
-
Combination of pembrolizumab, carboplatin, and paclitaxel or nab-paclitaxel
-
Squamous cell carcinoma and PD-L1 1% to 49%:
-
A combination of pembrolizumab, carboplatin, and paclitaxel or nab-paclitaxel should be recommended when it is possible.
-
For people who cannot receive immunotherapy, a combination of 2 chemotherapy drugs is recommended.
-
Combination of nivolumab and ipilimumab
-
Nivolumab and ipilimumab plus platinum-based chemotherapy
-
Cemiplimab plus chemotherapy
-
Durvalumab and tremelimumab plus platinum-based chemotherapy
-
For people who cannot receive pembrolizumab plus platinum chemotherapy, pembrolizumab alone may be recommended
-
Squamous cell carcinoma and PD-L1 less than 1%:
-
A combination of pembrolizumab, carboplatin, and paclitaxel or nab-paclitaxel should be recommended when it is possible.
-
In people who cannot receive immunotherapy, a combination of 2 chemotherapy drugs is recommended.
-
Combination of nivolumab and ipilimumab
-
Nivolumab and ipilimumab plus platinum-based chemotherapy
-
Cemiplimab plus chemotherapy
-
Durvalumab and tremelimumab plus platinum-based chemotherapy
-
EGFR gene mutations. Treatments with targeted therapies called TKIs may be options. Treatment with TKIs with or without chemotherapy may also be offered to certain patients as well as chemotherapy combinations with or without bevacizumab.
-
Osimertinib
-
Dacomitinib
-
Afatinib
-
Erlotinib
-
Erlotinib and ramucirumab
-
Gefitinib
-
Icotinib (Conmana; this is not approved in United States)
-
Amivantamab (Exon 20 mutations only)
-
ALK fusions. Treatments with targeted therapies called TKIs may be options. Targeted therapy options are alectinib, brigatinib, lorlatinib, ceritinib, or crizotinib.
-
ROS1 fusions. Treatments with targeted therapies called TKIs may be options. Targeted therapy options are entrectinib, crizotinib, or chemotherapy with or without immunotherapy.
-
BRAF V600E mutations. Treatments with targeted therapies called TKIs may be options. Targeted therapy options are dabrafenib and trametinib or chemotherapy with or without immunotherapy.
-
MET exon 14 skipping mutations. Treatments with targeted therapies called TKIs may be options. Targeted therapy options are capmatinib, tepotinib, or chemotherapy with or without immunotherapy.
-
RET fusions. Treatments with targeted therapies called TKIs may be options. Targeted therapy options are selpercatinib or pralsetinib (Gavreto). Chemotherapy with or without immunotherapy, bevacizumab, or both may also be recommended.
-
NTRK fusions. Treatments with targeted therapies called TKIs may be options. Targeted therapy options are entrectinib, larotrectinib, or chemotherapy with or without immunotherapy.
Second-line treatment. Second-line treatment for NSCLC depends on the gene mutations found in the tumor and the treatments patients have already received.
-
No changes in the EGFR, ALK, ROS1, BRAF, MET, RET, NTRK genes. If chemotherapy and immunotherapy were already given in the first line of treatment, then docetaxel with or without ramucirumab may be given in the second line. For people with non-squamous cell carcinoma, chemotherapy plus bevacizumab may be offered.
-
EGFR gene mutations. If osimertinib was not given in the first line, it could be given in the second line. If an EGFR inhibitor was already given, then chemotherapy with or without bevacizumab, immunotherapy, or both should be given.
-
ALK fusions. If crizotinib was already given, then the next treatment should be alectinib, brigatinib, or lorlatinib. If alectinib or brigatinib was already given, then the next treatment should be lorlatinib. If lorlatinib has already been given, then chemotherapy with or without immunotherapy, bevacizumab, or both should be given.
-
EGFR exon 20 insertion. Amivantamab (Rybrevant) can be used as a second-line treatment option for people with EGFR exon 20 insertion.
-
HER2 mutation. People who have a HER2 mutation and have received a previous systemic therapy may be offered trastuzumab deruxtecan.
-
RET fusions. If targeted therapy has not already been given, then selpercatinib or pralestinib may be offered. Otherwise, treatment options include chemotherapy with or without immunotherapy, bevacizumab, or both.
-
ROS1 fusions, BRAF V600E mutations, MET exon 14 skipping mutations, and NTRK fusions. If a TKI was already used in the first line, then chemotherapy with or without immunotherapy, bevacizumab, or both should be given.
-
KRAS G12C mutations. Sotorasib (Lumakras) or adagrasib (Krazati) can be used as a second-line treatment for people with KRAS G12C mutations.
Third-line treatment. Third-line treatment for NSCLC depends on the treatments that the patient has already received.
In all cases, patients and their doctors should discuss any reasons why some patients may not be able to receive immunotherapy and other treatment options described above.
This information is based in part on several ASCO recommendations for the treatment of lung cancer. Read more about these recommendations on the ASCO website.
Treatment for brain metastases
Chemotherapy is often not as effective as radiation therapy or surgery to treat NSCLC that has spread to the brain. For this reason, NSCLC that has spread to the brain is usually treated with radiation therapy, surgery, or both. This can cause side effects such as hair loss, fatigue, redness of the scalp, and problems with thinking, memory, and attention. With a small tumor, a type of radiation therapy called stereotactic radiosurgery can focus the radiation only on the tumor in the brain and lessen the side effects.
Newer targeted therapies have shown that they can work well to treat brain metastases. In those with an EGFR mutation in the cancer and no symptoms from the brain metastases, treatment with osimertinib may be recommended. For those with an ALK translocation and no symptoms from the brain metastases, treatment with alectinib, brigatinib, or ceritinib may be recommended. Similarly, targeted therapies that can penetrate into the brain can be used in other settings and subtypes of lung cancer that have other actionable targetable mutations, such as RET, ROS1, MET exon 14, and others. This may allow many patients to have a systemic therapy for brain metastases and avoid or delay the side effects that are associated with surgery or radiation therapy to the brain.
Below is a general summary of when and how surgery and radiation therapy are used to treat brain metastases:
-
People with 1 to 3 brain metastases generally receive stereotactic radiosurgery (SRS). If the brain metastases are large or causing symptoms due to pressure on the brain and the person is in general good health, they often receive surgery, followed by stereotactic radiation therapy.
-
Treatment for people in relatively good health and with more than 4 tumors that cannot be removed with surgery or more than 2 tumors that were removed surgically may include stereotactic radiation therapy or whole brain radiation therapy.
-
People who also have metastatic cancer in parts of the body other than the brain usually continue their treatment regimen if the disease outside the brain is not worsening. If the disease is worsening, the treatment plan may be changed based on the recommendations for that type of metastatic cancer.
The information in this section is based on a joint guideline from ASCO, the Society for Neuro-Oncology (SNO), and the American Society for Radiation Oncology (ASTRO), “Treatment for Brain Metastases.” Please note that this link takes you to a different ASCO website.
Learn about caring for someone with cancer that has spread to the brain.
Palliative and supportive care
As described above, palliative and supportive care will also be important to help relieve symptoms and side effects. Radiation therapy or surgery may also be used to treat metastases that are causing pain or other symptoms. Bone metastases that weaken major bones can be treated with surgery, and the bones can be reinforced using metal implants.
For most people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence). Most often, when there is recurrence, it is stage IV disease.
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above such as surgery, chemotherapy, and radiation therapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent NSCLC. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Return to top
If treatment does not work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.