A colonoscopy is a way for your doctor to see the part of your digestive system called the large intestine, or colon.
A colonoscopy is a medical test to help find potential problems, such as colorectal cancer or polyps. Polyps are small growths. They are not cancer, but they can turn into cancer. You might also have this test to look for the cause of bowel problems, including bleeding, a change in bowel movements, or other problems.
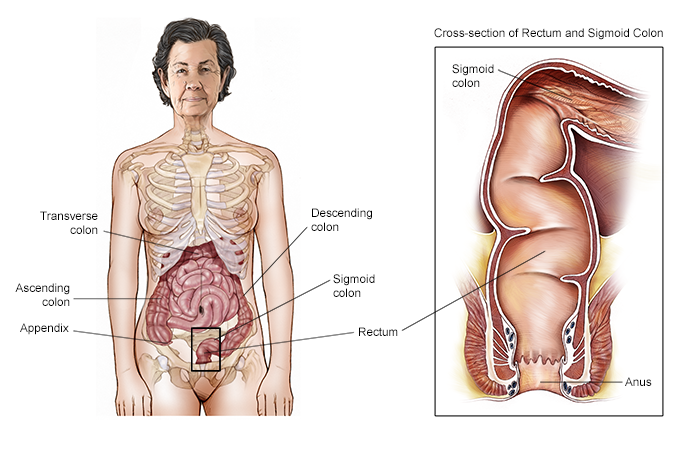
About the large intestine and colon
The large intestine is a major part of your digestive system, also called your gastrointestinal (GI) system. Your large intestine helps your body process waste. This is the food your body cannot use.
The colon is the biggest part of your large intestine. It empties into the rectum, where waste collects as bowel movements. These leave the body through the anus.
The drawing below shows the different parts of the colon and rectum.
How does a colonoscopy work?
This test uses a thin, flexible tube with a light and camera on one end. Your doctor will pass the tube into the rectum and then into the colon. Using the camera and light, the doctor will look at the inside of your colon. Another instrument will be inserted to remove any polyps or other tissue for a biopsy. During this procedure, you will receive a sedative and pain medication to make you more comfortable.
Who will do my colonoscopy?
A doctor specializing in the digestive system usually does a colonoscopy. This doctor is called a gastroenterologist or a GI specialist. Colonoscopies can also be done by surgeons, family practice doctors, physician assistants, or nurse practitioners. A nurse will probably help with the test, and an anesthesia specialist may be present as well.
How should I get ready for my colonoscopy?
When you schedule your colonoscopy, your doctor's office will tell you how to get ready. Be sure to follow their instructions carefully to avoid affecting the test results. Talk with the staff about the following topics, and ask questions beforehand about any information that is unclear or concerning to you.
Getting ready is especially important for a colonoscopy, because your colon needs to be as clean as possible. This lets your doctor see well into the colon.
Here are some things to remember:
What to eat. You will need to avoid solid food for 1 to 3 days before the test. You may drink clear liquids up until a certain time set by your health care team. Clear liquids may include fat-free bouillon or broth, black coffee, strained fruit juice, and gelatin.
Empty your colon. Your colon must be as empty as possible for the doctor to examine it. You will need an enema or strong laxatives before the test. Be sure to follow your doctor's instructions. You will take this the night before or the same day as the test.
If your doctor prescribes a laxative, it will be a pill or powder you mix with water before drinking. Once you take it, you will have bowel movements often until your colon is empty. Make sure you are near a bathroom during this time.
What to wear. You do not need to wear anything special to your appointment. You will need to change into a hospital gown once you arrive for the test. It is usually recommended to leave jewelry and other valuables at home.
Your medications and health history. Ask if you should take your usual medications on the day of the test. This includes any prescription drugs, over-the-counter drugs, and supplements. You may need to stop taking medications that increase your risk of bleeding for a few days before the test. These medications include aspirin and other blood thinners. Also, let your health provider know if you have any medical conditions or if you are pregnant.
Allergies. Let the medical staff know about any allergies to drugs, latex, or other things you have before the test.
Insurance, cost, and consent. If you are concerned about the cost of your test, contact your insurance company beforehand. Ask how much of the cost you will have to pay of your colonoscopy.
When you arrive for your test, you will be asked to sign a consent form. This form says you understand the benefits and risks of the procedure and agree to have it. Be sure to ask the health care team about any questions or concerns you have.
What happens during a colonoscopy?
A colonoscopy takes about 30 to 60 minutes.
When you get to the hospital or doctor's office, you will change into a hospital gown. You will be in a private room with a sheet draped over your body. You will be asked to lie on your side.
The nurse or anesthesia specialist will give you pain medication and a sedative. You will get this through an intravenous tube, or IV. The IV goes in a vein in your arm. You might feel a small sting from the IV needle when it goes in.
To start the colonoscopy, the doctor blows some air through the small tube into your colon. This inflates the colon slightly so the doctor can see better. You might need to change your position occasionally during the test. This is to help the doctor move the colonoscopy tube or get a better view. If you are asleep, the doctor or nurse will help with this.
If you have an abnormal growth, or polyp, in your colon, the doctor will remove it. Or they may take a small sample of tissue. This is not usually painful, and the doctor will stop any bleeding. If the growth is too large or complicated to remove during the colonoscopy, doctors may remove it later.
There is a small risk that the tube used for a colonoscopy might puncture the colon. This is rare, but you might need surgery to repair it if this happens. Talk with your health care team if you have concerns about this.
Is a colonoscopy painful?
There are two types of anesthesia that are usually used during a colonoscopy. Conscious sedation reduces pain and makes you less aware of things around you. You may be able to talk and respond to questions, or you might fall asleep. This is the most common type of sedation used for a colonoscopy.
If you have conscious sedation, you may feel some discomfort during a colonoscopy from lying still for a long time. You may also have some cramps. If so, tell your nurse or doctor. You may be able to change your position. Or, the health provider doing the colonoscopy may be able to adjust the tools to relieve the discomfort.
For some people who cannot take the drugs used for conscious sedation, such as due to other health conditions, deep sedation may be used. You will be monitored by an anesthesiologist or a nurse anesthetist during the procedure. If you have deep sedation, you will not be aware of the colonoscopy taking place. Learn more about anesthesia in another article on this website.
Some people choose to have no sedation during a colonoscopy. This is uncommon in the United States, but it is an option for this kind of procedure. Outside the United States, it is more common to have a colonoscopy without any sedation. Most people only experience mild discomfort during a colonoscopy, even without any sedation. But you should let your doctor or other health care provider know if you experience more discomfort or any pain during your colonoscopy.
What happens after a colonoscopy?
If you had anesthesia, you will stay at the hospital or doctor's office until you are completely awake. You should not drive a vehicle, operate machines, or make important decisions the rest of the day. Arrange ahead of time for a friend or family member to drive you home. You can expect to go back to normal activities the next day.
You may have cramps or feel bloated right after your colonoscopy. This usually goes away in a few hours. You might pass gas and even have some diarrhea as you release air from your colon.
You might notice a small amount of bleeding from your rectum. This is normal. However, call your doctor if you continue bleeding or if you have blood clots.
You should also contact your doctor immediately if you have:
-
Severe abdominal (belly) pain
-
A fever of 100 F (37.8 C) or higher
-
Bloody bowel movements
-
Dizziness
-
Weakness
A colonoscopy is a common and useful test to find and prevent GI problems. Be sure to ask your health care team about why this test is recommended for you and other questions on your mind. This can help you feel more comfortable before, during, and after having this test.
Questions to ask your health care team
Before your colonoscopy, you might want to ask your health care team these questions:
-
Why do you recommend that I have a colonoscopy?
-
What will happen if I do not have one?
-
Who will perform the colonoscopy? Where?
-
What will happen during the procedure?
-
How long will this test take?
-
Will I be awake during the colonoscopy?
-
What medication will I get to be more relaxed and comfortable?
-
What are the possible risks and benefits of a colonoscopy?
-
Can I take my regular medications the day of the procedure? Which ones should I not take? When can I take them again?
-
How else will I need to prepare for having this test, such as dietary instructions?
-
How do I find out what the procedure will cost me?
-
Will I need to avoid any activities after the colonoscopy, such as driving?
-
When will I learn the results? Who will explain the results to me?
-
Could I need more tests after my colonoscopy?
-
How often should I get a colonoscopy?
Recursos relacionados
Más información
American College of Gastroenterology: Colonoscopy
National Institute of Diabetes and Digestive and Kidney Diseases: Colonoscopy
