ON THIS PAGE: You will learn about the different types of treatments doctors use for people with pancreatic cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for pancreatic cancer. “Standard of care” means the best treatments known. These are the treatments that have been shown to be most effective based on evidence-based research conducted in clinical trials on a certain subset of patients. Information in this section is based on medical standards of care for pancreatic cancer in the United States. Treatment options can vary from one place to another.
When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials offer additional options to consider. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How pancreatic cancer is treated
In cancer care, different types of doctors who specialize in cancer, called oncologists, and other health care professionals often work together to create a patient’s overall care and treatment plan that combines different types of treatments and palliative and supportive care. This is called a multidisciplinary team. Cancer care teams include other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, patient navigators, social workers, pharmacists, counselors, dietitians, physical therapists, occupational therapists, and others. Learn more about the clinicians who provide cancer care.
Treatment options and recommendations depend on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of conversations are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is important for pancreatic cancer because there are different treatment options. Learn more about making treatment decisions.
When detected at an early stage, pancreatic cancer has a much higher chance of being successfully treated. However, there are also treatments that can help control the disease for patients with later stage pancreatic cancer to help them live longer and more comfortably.
The common types of treatments used for pancreatic cancer are described below, followed by a general outline of treatments by stage. Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
READ MORE BELOW:
Surgery
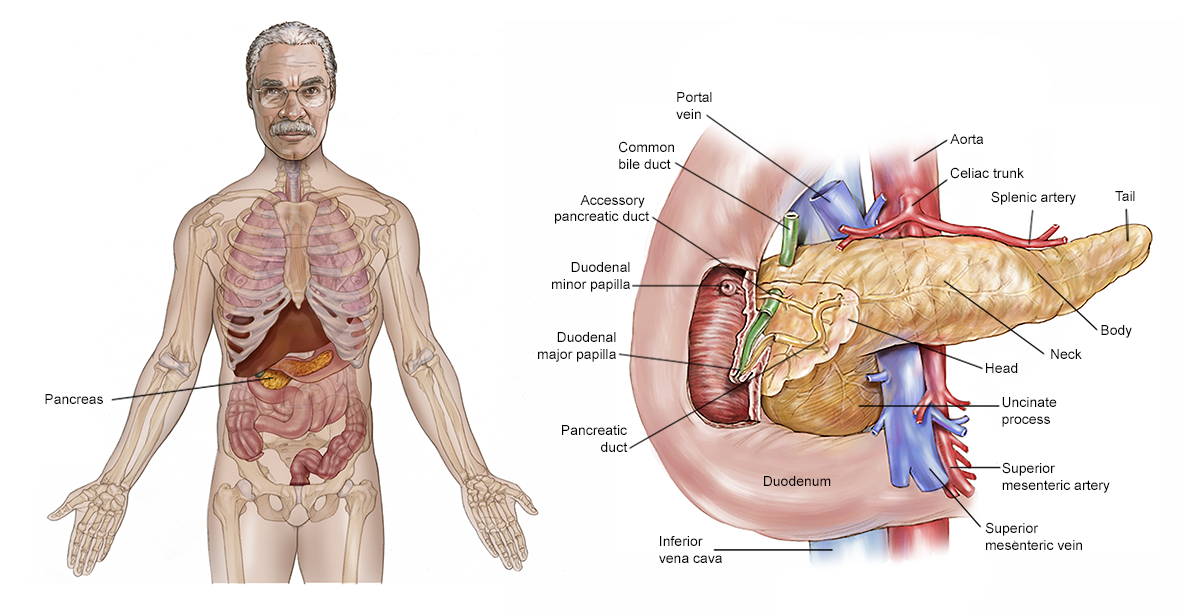
Surgery for pancreatic cancer includes removing all or part of the pancreas, depending on the location and size of the tumor in the pancreas. An area of healthy tissue around the tumor is also often removed. This is called a margin. A goal of surgery is to have “clear margins” or “negative margins,” which means that there are no cancer cells in the edges of the healthy tissue removed. A surgical oncologist is a doctor who specializes in treating cancer using surgery.
About 20% of people diagnosed with pancreatic cancer are able to have surgery because most pancreatic cancers are found after the disease has already spread. When surgery is a potential treatment option, there are many things to think about before a surgery of this type. It's important to have a thorough discussion with your health care team, including a pancreatic surgical oncologist, before deciding on surgical treatment. This discussion should include talking about the benefits, risks, and recovery time of the specific surgery recommended for you. If surgery is not an option, you and your doctor will talk about other treatment options. It is common to seek a second opinion from a specialized surgical oncologist for less common cancers such as pancreatic cancer.
Surgery for pancreatic cancer may be combined with systemic therapy and/or radiation therapy (see below). Typically, these additional treatments are given after surgery, which is called adjuvant therapy. However, systemic therapy and/or radiation therapy may sometimes be used before surgery to shrink a tumor. This is called neoadjuvant therapy or pre-operative therapy. After neoadjuvant therapy, the tumor is re-staged before planning surgery. Re-staging is usually done with another computed tomography (CT) scan to look at the change in tumor size and what nearby structures and blood vessels it is affecting.
Different types of surgery are performed depending on the purpose of the surgery.
-
Laparoscopy. Sometimes, the surgeon may choose to start with a laparoscopy. During a laparoscopy, several small holes are made in the abdomen and a tiny camera is passed into the body while the patient receives anesthesia. Anesthesia is medication to help block the awareness of pain. During this surgery, the surgeon can find out if the cancer has spread to other parts of the abdomen. If it has, surgery to remove the primary tumor in the pancreas is generally not recommended.
-
Surgery to remove the tumor. Different types of surgery are used depending on where the tumor is located in the pancreas. In all of the surgeries discussed below, nearby lymph nodes are removed as part of the operation. More than 1 type of surgeon, as well as other specialists, will usually be involved in your surgery.
-
Whipple procedure. This surgery is also referred to as a pancreaticoduodenectomy. A Whipple procedure may be done if the cancer is located only in the head of the pancreas. This is an extensive surgery in which the surgeon removes the head of the pancreas and the part of the small intestine called the duodenum, as well as the bile duct and stomach, or sometimes just part of the stomach. Then, the surgeon reconnects the digestive tract and biliary system. Temporary drains are usually put in the abdomen to help it drain and assist with patient recovery. Drains are usually placed during surgery and remain in place after surgery to drain any leakage of pancreas juice to the outside of the body. Drains are left in place for a variable period based on the amount and nature of their output, but they can be removed while still in the hospital and can stay in place for up to 2 to 3 months. A surgeon with experience treating pancreatic cancer should perform this procedure. There are several variations of the Whipple procedure, such as standard, pylorus-preserving, and radical pancreaticoduodenectomy. Learn more about having this procedure in another article on this website.
-
Distal pancreatectomy. This surgery is commonly done if the cancer is located in the left side of the tail of the pancreas. In this surgery, the surgeon removes the tail and body of the pancreas, as well as the spleen.
-
Total pancreatectomy. If the cancer has spread throughout the pancreas or is located in many areas in the pancreas, a total pancreatectomy may be needed. A total pancreatectomy is the removal of the entire pancreas, part of the small intestine, a portion of the stomach, the common bile duct, the gallbladder, and the spleen.
Supportive surgery and palliative procedures are often recommended to help with symptoms impacting a patient’s quality of life. Examples of palliative procedures and surgery can include bypass surgery, stent placements, and nerve blocks to alleviate jaundice, nausea and vomiting, and tumor-associated pain.
After surgery, you will need to stay in the hospital. How long you will need to stay in the hospital for will be determined by the type of surgery you've had, but it can range from several days to several weeks or longer. It will also include an at-home rest and recovery plan. At-home rest could be for about a month or longer with full recovery expected to take about 2 months. Your health care team will work closely with you on your pre-surgery preparation plan and post-surgery recovery plan, including providing important exercise, drain management (when a drain is put in during surgery), mindfulness, and dietary and nutritional recommendations.
Side effects of surgery include weakness, tiredness, and pain for the first few weeks after the procedure. Other side effects caused by the removal of the pancreas sometimes include difficulty digesting food and diabetes from the loss of insulin produced by the pancreas. Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have and how they can be managed. For more information on relieving side effects, see the section entitled "Physical, emotional, social, and financial effects of cancer," below. Learn more about the basics of cancer surgery.
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. Learn more about the basics of radiation therapy.
External-beam radiation therapy is the type of radiation therapy used most often for pancreatic cancer. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. There are different ways that radiation therapy can be given:
-
Traditional radiation therapy. This is also called conventional or standard fraction radiation therapy. It is made up of daily treatments of lower doses of radiation per fraction or day. It is given over 5 to 6 weeks in total and is generally given during the week with weekends off from treatment.
-
Stereotactic body radiation (SBRT) or cyberknife. These are shorter treatments of higher doses of radiation therapy given over as few as 5 days. This is a newer type of radiation therapy that can provide more localized treatment in fewer treatment sessions. Whether this approach works as well as traditional radiation therapy is not yet known, and it may not be appropriate for every person. It should only be given in specialized centers that have experience and expertise in using this technology for pancreatic cancer and identifying who it will work best for.
-
Proton beam therapy. This is a type of external-beam radiation therapy that uses protons rather than x-rays. At high energy, protons can destroy cancer cells. This type of therapy also lessens the amount of healthy tissue that receives radiation. Proton beam therapy may be given for a standard amount of time or for a shorter time like SBRT. It is not yet known whether it works better than standard radiation therapy, and it may not be an option for every person. It should be given in treatment centers that have the experience and skills needed to use this treatment for pancreatic cancer, which may only be available through a clinical trial.
Other types of radiation therapy may also be offered. There are many different ways radiation therapy is given, so it's important to talk with your doctor about their planned approach.
Often, chemotherapy (see below) will be given at the same time as radiation therapy because it can enhance the effects of the radiation therapy, which is called radiosensitization. Combining chemotherapy and radiation therapy may occasionally help shrink the tumor enough so it can be removed by surgery. However, chemotherapy given at the same time as radiation therapy often has to be given at lower doses than when given alone.
Radiation therapy may be helpful for reducing the risk of the pancreatic cancer returning or re-growing in the original location. However, there remains much uncertainty as to how much, if at all, it lengthens a person’s life.
Side effects from radiation therapy may include fatigue, mild skin reactions, nausea, upset stomach, and loose bowel movements. Most side effects go away soon after treatment is finished. Talk with your health care team about what you can expect and how side effects will be managed.
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication. Medications are often given through an intravenous (IV) tube placed into a vein using a needle, or occasionally as a pill or capsule that is swallowed (orally). If you are given oral medications to take at home, be sure to ask your health care team about how to safely store and handle them and whether they may interact with any of your other medications.
Chemotherapy is the main type of systemic therapy used for pancreatic cancer. However, targeted therapy and immunotherapy are occasionally used and are being studied as potential treatments for certain individuals when test results show specific molecular or genetic features (see Latest Research). Each of these types of therapies are discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Chemotherapy (updated 02/2024)
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. There is usually a rest period in between cycles. A patient may receive 1 drug at a time or a combination of different drugs given at the same time. The following drugs are approved by the U.S. Food and Drug Administration (FDA) for pancreatic cancer:
Combination treatments are usually best for people who are able to carry out their usual activities of daily living without help. This is because there are generally more side effects when 2 or more drugs are used together.
The choice of which combination to use varies depending on a variety of factors about which is most appropriate for the patient, such as their specific diagnosis, stage of disease, treatment history, genetics, side effects, and overall health. For pancreatic cancer, chemotherapy may be described by when and how it is given:
-
First-line chemotherapy. This is generally the first treatment used for people with either locally advanced or metastatic pancreatic cancer who have not received prior treatment (see Stages). The 2 most common first-line chemotherapy combinations used for pancreatic cancer are (1) FOLFIRINOX (5-FU, leucovorin, irinotecan, and oxaliplatin) and (2) gemcitabine plus nab-paclitaxel. In 2024, the FDA also approved NALIRIFOX (a combination very similar to FOLFIRINOX that uses nanoliposomal irinotecan instead of irinotecan) as an additional option for first-line treatment.
-
Second-line chemotherapy. If the first treatment does not work or stops working to control cancer growth, the cancer is called "refractory." Sometimes, first-line treatment does not work at all, which is called primary resistance. Or, treatment may work well for a while and then stop being effective later, which is sometimes called secondary or acquired resistance. In these situations, patients may benefit from additional treatment with different drugs if the patient’s overall health is good. There is significant ongoing research focused on developing other new treatments for second-line, as well as third-line, treatment and beyond. Some of these treatments have shown considerable promise (see the Latest Research section).
-
Off-label use. This refers to a drug being given for a condition not listed on its label. This means that the drug is not being given for the condition(s) that the drug is specifically approved for by the FDA. It can also mean that the drug is being given differently than the instructions on the label. An example of this is if a doctor wants to use a drug only approved for breast cancer to treat pancreatic cancer. Using a drug off-label is only recommended when there is solid evidence that the drug may work for another disease not included on the label. This evidence may include previously published research, promising results from ongoing research, or results from biomarker testing of the tumor that suggest the drug may work. However, off-label use of drugs may not be covered by your health insurance provider. Exceptions are possible, but it is important that you and/or your health care team talk with your insurance provider before this type of treatment begins.
Side effects of chemotherapy
The side effects of chemotherapy depend on which drugs you receive. In addition, not all patients have the same side effects even when given the same drug. Side effects in general can include poor appetite, nausea, vomiting, diarrhea, gastrointestinal problems, rash, mouth sores, hair loss, and a lack of energy. People receiving chemotherapy are also more likely to have low levels of white blood cells, red blood cells, and platelets, which give them a higher risk of anemia, infections, and bruising and bleeding easily.
Certain drugs used in pancreatic cancer are also linked with specific side effects. For example, capecitabine can cause redness and discomfort on the palms of the hands and the soles of the feet. This condition is called hand-foot syndrome. Both oxaliplatin and nab-paclitaxel can cause numbness and tingling in the fingers and toes, called peripheral neuropathy. Peripheral neuropathy is a side effect of nab-paclitaxel as well. These are examples, and it is important to talk with your doctor beforehand about side effects of the cancer medication(s) recommended for you.
Most side effects typically go away between treatments and after the treatments have ended, but some can be longer-lasting and can worsen as treatment continues. Your doctor can suggest ways to relieve these side effects. If the side effects are severe, your doctor may reduce the chemotherapy dose or pause chemotherapy for a short time.
Learn about the basics of chemotherapy.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them.
-
Erlotinib (Tarceva). This drug is approved by the FDA for people with advanced pancreatic cancer in combination with the chemotherapy drug gemcitabine. Erlotinib blocks the effect of the epidermal growth factor receptor (EGFR), a protein that can become abnormal and help cancer grow and spread. This drug is taken as a pill orally by mouth, usually once a day. The side effects of erlotinib include a skin rash similar to acne, diarrhea, loss of appetite, and fatigue. This drug is not commonly used anymore due to its relatively modest benefit and the development of more effective therapies but is an option.
-
Olaparib (Lynparza). This drug is approved for people with metastatic pancreatic cancer associated with a germline (hereditary) BRCA mutation. It is intended for use as maintenance therapy after a patient has been on platinum-based chemotherapy, such as oxaliplatin or cisplatin, for at least 16 weeks with no evidence of disease progression. This drug is taken as a pill orally by mouth, usually twice a day. Common side effects from this drug can include nausea, vomiting, diarrhea or constipation, fatigue, feeling dizzy, loss of appetite, taste changes, low red blood cell counts, low white blood cell counts, belly pain, and muscle and joint pain.
-
Tumor-agnostic treatments. These refer to drugs that can be used for any type of cancer that has a specific genetic change, regardless of where the cancer started. These genetic changes tend to be rare in pancreatic cancer. When applicable, these drugs can be given to treat patients with pancreatic cancer that is metastatic or locally advanced that has not responded to chemotherapy. Examples of these drugs include:
-
Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek). These drugs are for tumors that have a particular genetic change called an NTRK fusion (see Diagnosis). They are taken as pills orally by mouth. Common side effects can include dizziness, fatigue, nausea, vomiting, constipation, weight gain, and diarrhea.
-
Selpercatinib (Retevmo). This drug is used for tumors that have a RET fusion. Common side effects of this pill include fluid retention, diarrhea, fatigue, dry mouth, high blood pressure, abdominal pain, constipation, rash, nausea, and headache.
-
Dabrafenib plus trametinib. This combination of 2 different pills is used for tumors that have BRAF V600E mutations. Common side effects include fever, fatigue, nausea, rash, chills, headache, bleeding, cough, vomiting, constipation, diarrhea, muscle and joint aches, and fluid retention.
Other targeted therapies can sometimes be considered for off-label use (see above) if molecular testing of the tumor shows the presence of certain rare mutations or genetic changes that suggest possible benefit, such as sotarasib (Lumakras) or adagrasib (Krazati) for tumors with KRAS G12C mutations.
Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Learn more about the basics of targeted treatments.
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells.
Immune checkpoint inhibitors, which include anti-PD-1 antibodies such as pembrolizumab (Keytruda) and dostarlimab (Jemperli), are an option for treating pancreatic cancers that have high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), or high tumor mutational burden (TMB) (see Diagnosis). Approximately 1% to 1.5% of pancreatic cancers are associated with high MSI-H.
Immunotherapy, combined with chemotherapy, is also being studied as part of emerging clinical trials.
Different types of immunotherapy can cause different side effects. Talk with your doctor about possible side effects of the immunotherapy recommended for you. Learn more about the basics of immunotherapy.
Return to top
Physical, emotional, social, and financial effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative and supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative and supportive care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative and supportive care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments, such as chemotherapy, surgery, or radiation therapy, to improve symptoms. Palliative and supportive care should not be confused with hospice care, which is used when a cure is not likely or when people are in the last months of life.
Before treatment begins, talk with your health care team about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative and supportive care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
Cancer care is often expensive, and navigating health insurance can be difficult. Ask your doctor or another member of your health care team about talking with a financial navigator or counselor who may be able to help with your financial concerns.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of monitoring and tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Palliative and supportive care for people with pancreatic cancer may include:
-
Palliative chemotherapy. Any chemotherapy regimen discussed above may help relieve the symptoms of pancreatic cancer, such as lessening pain, improving a patient’s energy and appetite, and stopping or slowing weight loss. This approach is used when the cancer has spread and cannot be cured, but the symptoms of the cancer can be improved with chemotherapy. When making decisions about palliative chemotherapy, it is important that you and your doctor weigh the benefits with the possible side effects and consider how each treatment might affect your quality of life.
-
Relieving bile duct or small intestine blockage. If the tumor is blocking the common bile duct or small intestine, placing a tiny tube called a stent can help keep the blocked area open. This procedure can be performed using nonsurgical approaches, such as endoscopic retrograde cholangiopancreatography (ERCP), percutaneous transhepatic cholangiography (PTC), or endoscopy (see Diagnosis). A stent can be either plastic or metal. The type used depends on the availability, insurance coverage/cost, a person’s expected lifespan, and whether the cancer will eventually be removed with surgery. In general, plastic stents are less expensive and are easier to insert and remove. However, they need to be replaced every few months, are associated with more infections, and are more likely to move out of place. Stents are typically placed inside the body, but sometimes, a tube may need to be placed through a hole in the skin of the abdomen to drain fluid, such as bile. This is called percutaneous drainage. Sometimes, a patient may need surgery to create a bypass and alleviate symptoms, even if the tumor itself cannot be completely removed.
-
Improving digestion and appetite. A special diet, medications, and specially prescribed enzymes may help a person digest food better if their pancreas is not working well or has been partially or entirely removed. Meeting with a dietitian/nutritionist is recommended for most patients, especially for those who are losing weight and have a poor appetite because of the disease. Daily exercise is highly recommended, and your doctor can work with you on an appropriate regimen.
-
Controlling diabetes. Insulin will usually be recommended if a person develops diabetes due to the loss of insulin produced by the pancreas, which is more common after a total pancreatectomy. Your health care team will help you with monitoring and controlling this condition.
-
Relieving pain and other side effects. Morphine-like drugs called opioid analgesics are often needed to help reduce pain. Special types of nerve blocks done by pain specialists may also be used. One type of nerve block is a celiac plexus block, which helps relieve abdominal or back pain. During a nerve block, the nerves are injected with either an anesthetic to stop pain for a short time or a medication that destroys the nerves and can relieve pain for a longer time. A nerve block can be performed either percutaneously (through the skin) or with an endoscopic ultrasound (see above). Depending on where the tumor is located, radiation therapy can sometimes be used to relieve pain. Learn more about managing pain.
Recommended palliative and supportive care may also include complementary therapies. It is important that you talk with your doctor before trying any complementary therapies to make sure they do not interfere with your other cancer treatments.
Palliative and supportive care is not limited to managing a patient’s physical symptoms. There may also also emotional issues, like anxiety or depression, and psychological issues that many patients experience that can be managed with professional help and support. A professional can help with developing coping skills and the overall difficulty of dealing with cancer. Cancer also affects caregivers and loved ones, and they are encouraged to seek out support as well.
Return to top
Treatment options by stage of pancreatic cancer
Different treatments may be recommended for each stage of pancreatic cancer. The general options by stage are described below. For more detailed descriptions, see “How pancreatic cancer is treated,” above. Your doctor will recommend a specific treatment plan for you based on your specific diagnosis and needs. Clinical trials may also be a treatment option for each stage.
Below are some of the possible treatments based on the stage of the cancer. The information below is based on American Society of Clinical Oncology (ASCO) guidelines for the treatment of pancreatic cancer. Your care plan may also include treatment for symptoms and side effects, an important part of pancreatic cancer care. Also, patients with any stage of pancreatic cancer are encouraged to consider clinical trials as a treatment option. Talk with your doctor about all of your treatment options. Your doctor will have the best information about which treatment plan is recommended for you.
Potentially curable pancreatic cancer (also called resectable and borderline resectable pancreatic cancer)
-
Surgery
-
Treatment before surgery, also called neoadjuvant therapy or pre-operative therapy
-
Chemotherapy, with or without radiation therapy, is regularly used for patients with borderline resectable pancreatic cancer. It is done to try to shrink the tumor and increase the chance that the surgeon can remove the tumor with clear margins. Even for people with resectable pancreatic cancer, neoadjuvant therapy is also sometimes recommended.
-
Treatment after surgery, also called adjuvant therapy or post-operative therapy
-
Adjuvant chemotherapy usually starts within 4 to 12 weeks after surgery depending on how quickly a patient recovers. It is typically given for a total of 6 months. The type of combination chemotherapy given is usually FOLFIRINOX (5-FU, leucovorin, irinotecan, and oxaliplatin) for those patients who have recovered well from surgery and are healthy enough for a multidrug combination. The alternative option is gemcitabine, either as a single drug or in combination with a second drug called capecitabine. Multidrug combinations have been shown to be more effective than just gemcitabine alone, but are associated with more side effects, including diarrhea, fatigue, neuropathy, low levels of white blood cells, and hand-foot syndrome. Talk with your doctor about the best chemotherapy options for you.
-
The role of radiation therapy after surgery remains controversial. The option to use radiation therapy after surgery depends on each patient’s situation. For example, it may be an option for when there were not clear margins after surgery.
-
For patients who received treatment before surgery, the need for additional treatment after surgery depends on each patient’s situation and overall health.
Locally advanced pancreatic cancer
-
First-line therapy
-
Chemotherapy with a combination of drugs may be an option depending on each patient’s situation and overall health (see options listed under "Metastatic pancreatic cancer" below).
-
Radiation therapy may also be an option. It is used most often after chemotherapy when the cancer has not spread beyond the pancreas. The choice of the type of radiation therapy used, such as standard external beam or SBRT (see "Radiation therapy" above), depends on several factors, including the size and location of the tumor.
-
Second-line therapy
-
Clinical trials
Metastatic pancreatic cancer
If cancer spreads to another part in the body from where it started, it is referred to as metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option, so talk with your doctor about clinical trials for which you may be eligible. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
Your treatment plan may include a combination of the treatments discussed above. Treatment options for people with metastatic pancreatic cancer depend heavily on a patient’s overall health, preferences, and support system.
Information below is based on the ASCO guideline, “Metastatic Pancreatic Cancer.” Please note that this link takes you to another ASCO website.
Depending on factors such as your preferences, characteristics, and your comorbidity profile, first-line options include:
-
Chemotherapy with a combination of fluorouracil, leucovorin, irinotecan, and oxaliplatin, called FOLFIRINOX.
-
Gemcitabine plus nab-paclitaxel.
-
Gemcitabine by itself for patients who are not healthy enough for the more aggressive 2 combinations above.
-
Occasionally, another gemcitabine-based or fluorouracil-based combination may be used, such as gemcitabine plus cisplatin, gemcitabine plus capecitabine, or FOLFOX.
Second-line options include those listed below. These are generally for when the disease worsens or patients experienced severe side effects during first-line therapy.
-
Fluorouracil alone or combined with nanoliposomal irinotecan, irinotecan, or oxaliplatin may be recommended based on the overall health of the patient and shared decision-making.
-
Gemcitabine alone or in combination with nab-paclitaxel may be offered.
-
Pembrolizumab or dostarlimab is recommended when the cancer has high microsatellite instability (MSI-high) or mismatch repair deficiency (dMMR). It is important to note that only about 1 to 1.5% of people with pancreatic cancer have MSI-high disease. Patients whose tumors show high tumor mutational burden (TMB) are also candidates to receive pembrolizumab.
-
Certain oral targeted therapies can be used for patients whose tumors have rare genetic changes, including larotrectinib or entrectinib for cancers with an NTRK fusion; selpercatinib for cancers with a RET fusion; and the combination of dabrafenib plus trametinib for cancers with a BRAF V600E mutation.
-
Patients who have an inherited BRCA1 or BRCA2 mutation and who have received first-line platinum-based chemotherapy that stopped the cancer from growing or spreading for 16 weeks or more may continue treatment with chemotherapy or receive maintenance therapy with olaparib, a targeted therapy. Maintenance therapy is treatment with the goal of keeping the cancer in remission, and it is an option after shared decision-making between the patient and doctor.
Maintenance therapy can also be an option for patients whose disease has not progressed on first-line treatment, but who, due to side effects, may no longer be able to continue with their original treatment. The only approved maintenance therapy is olaparib, which is beneficial in people who have metastatic pancreatic cancer associated with a germline (hereditary) BRCA mutation following first-line platinum-based chemotherapy. For other patients, maintenance therapy might mean simplifying their original chemotherapy regimen. For example, it might be simplified from gemcitabine/nab-paclitaxel to gemcitabine alone, or from FOLFIRINOX to FOLFOX, FOLFIRI, or capecitabine. Learn more about the basics of maintenance therapy.
Palliative and supportive care will also be important to help relieve symptoms and side effects. Talk with your doctor as early as possible about the symptoms you are experiencing, your mental well-being, and the social support available to you. Treatment to ease any cancer-related pain or other symptoms will be offered.
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. It is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the cancer returns after the original treatment, it is called recurrent cancer. Pancreatic cancer may come back in or near the pancreas (called a local or regional recurrence), or elsewhere in the body (called a distant recurrence, which is similar to metastatic disease).
If a recurrence happens, a new cycle of diagnostic testing will begin to learn as much as possible about the extent and location of it. After this testing is done, you and your doctor will talk about the treatment options. The treatment of recurrent pancreatic cancer is similar to the treatments described above and usually involves chemotherapy. Radiation therapy or surgery may also be used to help relieve symptoms. Your doctor may suggest clinical trials that are studying new ways to treat recurrent pancreatic cancer. Whichever treatment plan you choose, palliative and supportive care will be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Return to top
If treatment does not work
Recovery from pancreatic cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team and family and friends to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
Planning for your future care and putting your wishes in writing is important, especially at this stage of disease. Then, your health care team and loved ones will know what you want, even if you are unable to make these decisions. Learn more about putting your health care wishes in writing.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care, which is not the same as palliative and supportive care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with your doctor or a member of your palliative care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people want and need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.