ON THIS PAGE: You will learn about the different types of treatment doctors use for people with ovarian, fallopian tube, and peritoneal cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for ovarian, fallopian tube, and peritoneal cancer. Ovarian/fallopian tube epithelial cancers are treated the same way. “Standard of care” means the best treatments known. Information in this section is based on medical standards of care for ovarian/fallopian tube cancer in the United States. Treatment options can vary from one place to another.
Clinical trials may also be an option for you, which is something you can discuss with your doctor. A clinical trial is a research study that tests a new approach to treatment. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How ovarian/fallopian tube cancer is treated
In cancer care, different types of doctors who specialize in cancer, called oncologists, work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. Cancer care teams include other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, physical therapists, occupational therapists, and others. Learn more about the clinicians who provide cancer care.
Treatment options and recommendations depend on several factors, including the type, stage, and grade of the cancer, possible side effects, and the patient’s preferences and overall health or personal goals, such as the patient’s age and any plans to have children in the future.
Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of conversations are called "shared decision-making." Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is important for ovarian, fallopian tube, and peritoneal cancer because there are different treatment options. Learn more about making treatment decisions.
The common types of treatments used for ovarian/fallopian tube cancer are described below. Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
READ MORE BELOW
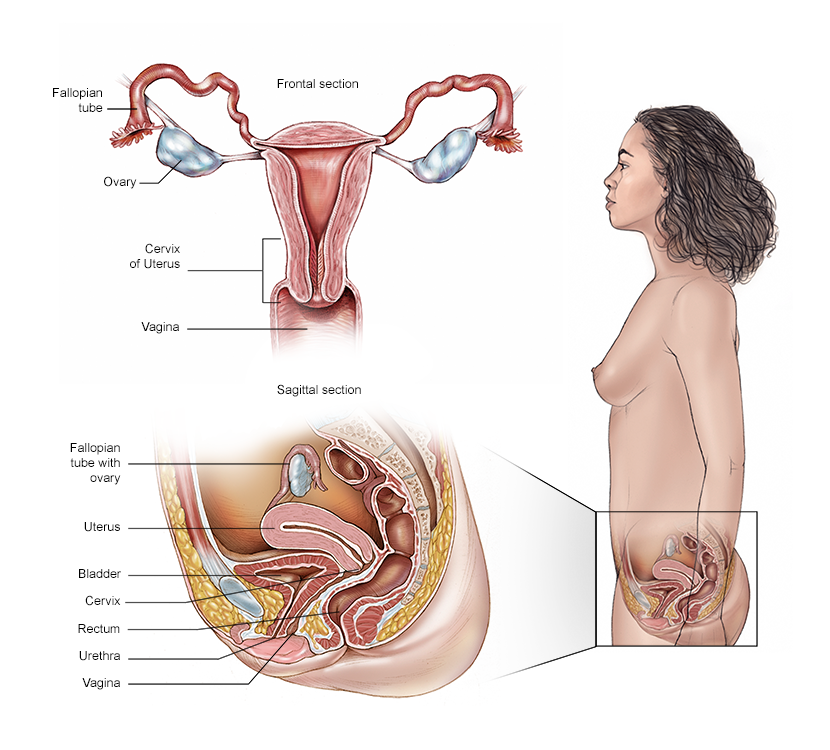
Concerns about sexual health and having children
Patients may have concerns about if or how their treatment may affect their sexual health and fertility. These topics should be discussed with the health care team before treatment begins.
If you still potentially want to be able to get pregnant in the future, talk with a reproductive endocrinologist (a doctor who is a fertility expert) before cancer treatment begins. It may be helpful to discuss what options for fertility preservation are covered by health insurance.
In addition to potential fertility concerns, cancer treatments such as surgery, radiation therapy, and chemotherapy can directly impact sexual health and function. Common post-treatment issues related to sexual function include decreased desire for sex (called libido), anxiety about sex, body image concerns, pain with intercourse, and/or vaginal dryness. These issues may feel difficult to discuss with your health care team, but sexual health is an important part of your overall health. Many treatments exist to help address these concerns, so talk with your doctor about what is recommended for you.
Return to top
Surgery
Surgery is an important treatment for these types of cancer. A gynecologic oncologist is a doctor who specializes in the treatment of gynecologic cancers, including surgery and medications such as chemotherapy (see "Chemotherapy," below).
As mentioned in Diagnosis, surgery is often needed to find out the complete extent of the disease. The goal is to provide an accurate stage. Minimally invasive surgery is often used to confirm a diagnosis and to determine if a debulking procedure (see below) should be done at the time of diagnosis or after chemotherapy has been given first. This is important because imaging tests aren’t always able to see the full extent of a disease.
For those patients whose cancer is confined to the ovary who proceed to have a debulking procedure, the surgery will also include a staging procedure that may involve the removal of various tissues, including lymph nodes, to see if there is evidence that the cancer has spread. For those patients with advanced cancer, removing as much of the cancer as possible is the goal. This procedure has been shown to provide the best benefit when combined with chemotherapy after surgery.
There are several surgical options for ovarian/fallopian tube cancer. The stage of the tumor determines the types of surgery recommended. Sometimes doctors perform 2 or more procedures during the same surgery:
-
Salpingo-oophorectomy. This surgery involves removal of the ovaries and fallopian tubes. If both ovaries and both fallopian tubes are removed, it is called a bilateral salpingo-oophorectomy. If the patient wants to become pregnant in the future and has early-stage cancer, it may be possible to remove only 1 ovary and 1 fallopian tube if the cancer is located in only 1 ovary. That surgery is called a unilateral salpingo-oophorectomy. For people with a germ cell type of ovarian tumor, often only the ovary with the tumor needs to be removed, preserving the ability to become pregnant.
-
Hysterectomy. This surgery focuses on the removal of the uterus and, if necessary, surrounding tissue. If only the uterus is removed, it is called a partial hysterectomy. A total hysterectomy is when both the uterus and cervix are removed.
-
Lymphadenectomy/lymph node dissection. During this procedure, the surgeon may remove lymph nodes in the pelvis and paraortic areas.
-
Omentectomy. This is surgery to remove the thin tissue that covers the stomach and intestines.
-
Cytoreductive/debulking surgery. This surgery is used for people with advanced ovarian/fallopian tube cancer. The goal of cytoreductive surgery is to remove as much tumor as is safely possible. This may include removing tissue from nearby organs, such as the spleen, liver, and part of the small bowel or colon. This may also involve removing part of each of these organs. This procedure can help reduce a person’s symptoms, as it removes masses that may be pressing on other organs. It may help increase the effectiveness of other treatment(s) given after surgery, such as chemotherapy, to control the disease that remains. If the disease has spread beyond the ovaries, fallopian tubes, or peritoneum, doctors may use chemotherapy to shrink the tumor before cytoreductive or debulking surgery. This is called neoadjuvant chemotherapy. Your doctor may recommend neoadjuvant chemotherapy if there is a large buildup of fluid in your abdomen or around your lungs, or if they think it would be safer and equally effective for you to have 2 to 3 cycles of chemotherapy prior to debulking surgery. Your doctor will discuss the reasons for neoadjuvant chemotherapy in your case. Your doctor may also administer chemotherapy during the time of surgery. A method for this is called hyperthermic intraperitoneal chemotherapy (HIPEC), which is being studied in clinical trials and is not currently the standard of care.
Debulking surgery should be performed by a board-certified gynecologic oncologist if possible. Talk with your doctor before surgery about the risks and benefits of this procedure. Ask about the surgeon’s experience with debulking surgery and whether the surgery will be performed in a minimally invasive way or by an open incision. Sometimes, the surgery can be done robotically. Talk with your doctor about the different surgical options.
Side effects of surgery
Surgery can cause mild or more severe side effects. It typically causes short-term pain and tenderness. If there is pain, the doctor will prescribe an appropriate medication. For several days after the operation, you may have difficulty emptying your bladder (urinating) and/or having bowel movements. Surgery can also cause more severe effects, including infection, bleeding, or injury to other organs.
If both ovaries are removed, pregnancy is no longer possible. The loss of both ovaries eliminates the body's source of sex hormones, resulting in early menopause, unless a person is already in menopause. Soon after surgery, a person is likely to have menopausal symptoms, including hot flashes and vaginal dryness.
Studies have shown that people who have their surgery performed by a gynecologic oncologist are more likely to be successfully treated with surgery and have fewer side effects. Free searchable databases to use to locate a doctor include ASCO's Find a Cancer Doctor database and The Foundation for Women's Cancer. (Please note this second link takes you to a different website.)
Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have. Learn more about the basics of cancer surgery.
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication, or a gynecologic oncologist. Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If given through a vein, the vein is often accessed through a port, which is a small plastic or metal disc placed under the skin before treatment begins. If you are given oral medications to take at home, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for ovarian, fallopian tube, and peritoneal cancer include:
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
-
Hormone therapy
Each of these types of therapies is discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if you are taking any other prescriptions or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases.
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells or by destroying the cancer cells.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or a combination of different drugs given at the same time. The type of the chemotherapy used depends on several factors. Patients may be given chemotherapy before or after surgery or as a primary treatment option.
If the chemotherapy stops or slows the cancer, then maintenance therapy with targeted treatments may be used for certain patients (see "Targeted therapy," below).
Neoadjuvant chemotherapy
Neoadjuvant chemotherapy is a medical term used to describe chemotherapy that is given before surgery. It is done to reduce the size of a tumor before surgery. It is usually started after a biopsy, so the doctors can determine where the tumor began. Neoadjuvant chemotherapy is usually given for 3 to 4 cycles before considering surgery, called interval surgery. This treatment usually consists of carboplatin (available as a generic drug) given intravenously with paclitaxel (Taxol) or other drugs. The typical treatment cycle is to be given these drugs every 3 weeks. Talk with your doctor about which scheduling option is best for your treatment plan.
In 2016, the American Society of Clinical Oncology (ASCO) and the Society of Gynecologic Oncology (SGO) released a joint clinical practice guideline on the use of neoadjuvant chemotherapy to treat newly diagnosed, advanced ovarian/fallopian tube cancer. Listen to a podcast about what this treatment guideline means for patients.
Adjuvant chemotherapy
Adjuvant chemotherapy is a medical term to describe chemotherapy that is given after surgery to destroy any remaining cancer. For these types of cancer, the specific drugs typically are carboplatin given with paclitaxel or other drugs intravenously (IV). Most of these drugs are given once every 3 weeks.
Another approach is called “dose-dense” chemotherapy. This is when paclitaxel is given weekly instead of every 3 weeks. Research studies have shown conflicting results on the effectiveness of this approach. Some studies show better outcomes with dose-dense chemotherapy, and others show that the outcomes are the same. Recent clinical trials in the United States and Europe did not show a benefit of dose-dense chemotherapy compared to chemotherapy given every 3 weeks, in contrast to a clinical trial from Japan.
Adjuvant chemotherapy can also be infused directly into the abdomen through a second port. This is called intraperitoneal or “IP” chemotherapy. This approach may be considered for people with stage III cancer after a debulking surgery that removes all visible disease. However, the effectiveness of IP chemotherapy is not clear. While some research studies have shown that IP treatment may offer more benefit than IV treatment in some patients, more recent research has shown no difference between IV and IP chemotherapy, especially when bevacizumab (Avastin) is added to the treatment.
A treatment plan that adds bevacizumab to adjuvant chemotherapy with carboplatin and paclitaxel, followed by a course of bevacizumab alone, was approved by the U.S. Food and Drug Administration (FDA) in 2018. Bevacizumab is a targeted therapy that stops blood vessel growth (see "Targeted therapy," below). This adjuvant treatment is approved for people with stage III or stage IV ovarian/fallopian tube/peritoneal cancer. In general, bevacizumab used for ovarian/fallopian tube cancer has prolonged the time before the cancer returns in some patients.
Talk with your doctor about which plan is best for your situation. With each of these approaches, doctors consider a variety of factors, such as age, kidney function, and other existing health problems before recommending a treatment schedule.
Side effects of chemotherapy
For ovarian, fallopian tube, and peritoneal cancer, the side effects of chemotherapy depend on the individual and the dose used. Side effects can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, peripheral neuropathy, and diarrhea. These side effects usually go away after treatment is finished, though some may persist after the completion of treatment, including peripheral neuropathy.
Another possible side effect of chemotherapy is having difficulty with concentration and memory. For example, the patient may have issues with attention span or memory, sometimes called “chemobrain.” Other possible side effects include losing the ability to become pregnant, called infertility, and early menopause. Rarely, certain drugs may cause some hearing loss or kidney damage. Patients may be given extra fluid intravenously to protect their kidneys. Before treatment begins, patients should talk with their health care team about possible short-term and long-term side effects of the specific drugs they will receive. It is important to note that many side effects can be reduced by adjusting the dose and/or schedule. Be sure to discuss any side effects you are experiencing with your doctor.
Learn more about the basics of chemotherapy.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments.
For ovarian/fallopian tube cancer, some targeted therapy drugs are directed at specific genes that might be found with abnormalities in certain types of epithelial ovarian/fallopian tube cancer. Standard chemotherapy has been effective in treating most ovarian/fallopian tube cancer. Typically, about 20% of high-grade tumors have mutations in the BRCA genes. Other tumor mutations are less common.
The BRCA mutation, even if found only in the tumor and not in the blood, may increase the effectiveness of certain classes of drugs, such as poly ADP-ribose polymerase (PARP) inhibitors (see below).
Other types of less common ovarian/fallopian tube cancers include low-grade serous, endometrioid, clear cell, and mucinous cancers. These tumors have a variety of mutations, including BRAF, PI3KCA, and PTEN, which means targeted treatment may be available.
-
PARP inhibitors. PARP inhibitors block an enzyme involved in repairing damaged DNA. By blocking this enzyme, DNA inside cancer cells may be less likely to be repaired, leading to cell death and possibly slowing down or stopping tumor growth. The BRCA genes (BRCA1 and BRCA2) are normally involved in DNA repair, and a mutation in these genes interferes with this pathway function. PARP inhibitors make it difficult for cells that otherwise have a BRCA mutation to grow and divide.
PARP inhibitors are also effective in people who do not have BRCA mutations, particularly in those who have cancer that has a deficiency in repairing DNA damage. This is called homologous recombination deficiency (HRD). This includes people with platinum-sensitive recurrent disease (see more below). There are tests that can be done to see if a tumor has evidence of HRD and the patient could benefit from treatment with a PARP inhibitor. PARP inhibitors may be used for maintenance therapy after first- or second-line platinum-based therapy and to treat recurrent cancer (see sections below). ASCO does not recommend that people with early-stage (stage I or II) epithelial ovarian cancer receive PARP inhibitors in combination with first platinum-based treatment. ASCO also does not recommend using PARP inhibitors more than once in the overall treatment plan. This is an active area of research. Talk with your doctor about the potential benefits and risks of PARP inhibitors.
-
Anti-angiogenesis inhibitors. Drugs called anti-angiogenesis inhibitors block the action of a protein called vascular endothelial growth factor (VEGF). These drugs have been shown to increase the cancer’s response to treatment and delay the time it takes for the cancer to return. VEGF promotes angiogenesis, which is the formation of new blood vessels. Because a tumor needs nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumor.
Bevacizumab, an antibody that binds VEGF and prevents it from being active, has been shown to be effective in treating ovarian/fallopian tube cancer. It may be combined with chemotherapy to treat stage III or stage IV disease (see "Chemotherapy," above). It is also used as a maintenance drug (see below).
-
Antibody-drug conjugates. Antibody-drug conjugates are a type of drug that use monoclonal antibodies to deliver an attached chemotherapy directly to cancer cells. A monoclonal antibody is a targeted therapy that recognizes and attaches to a specific protein and does not affect cells that do not have that protein.
In 2022, the FDA approved the antibody-drug conjugate mirvetuximab soravtansine-gynx (Elahere) to treat people with folate receptor alpha (FRα) positive, platinum-resistant epithelial ovarian, fallopian tube, or peritoneal cancer who have received 1 to 3 previous systemic treatments.
Maintenance therapy using targeted therapy (updated 09/2022)
Maintenance therapy is a medical term used to describe treatment that is used to reduce the risk of cancer coming back, called a recurrence, or to delay the time to recurrence. The drugs are used to “maintain” a clinical remission, which is when there is no evidence of disease or a marked reduction in disease after the course of chemotherapy treatment has been completed.
Targeted therapy is one option used to maintain remission in people whose ovarian/fallopian tube/peritoneal cancer has completely responded to the initial chemotherapy and the disease is in a complete or partial clinical remission.
Niraparib (Zejula), olaparib (Lynparza), and rucaparib (Rubraca) are PARP inhibitors approved by the FDA for use in maintenance therapy for ovarian/fallopian tube/peritoneal cancer. If the cancer has been slowed or put into remission by first-line platinum-based chemotherapy, ASCO recommends maintenance therapy with a PARP inhibitor for patients newly diagnosed with stage III or IV ovarian cancer that is either a high-grade serous cancer (HGSC) or endometrioid cancer. People who have a BRCA mutation should be offered olaparib, niraparib, or rucaparib as maintenance therapy and are the group for whom the greatest potential benefit from therapy with PARP inhibitors has been shown. For those who have cancer with HRD (see above), maintenance therapy with niraparib or rucaparib is an option. Niraparib or rucaparib may also be offered to people who do not have a BRCA mutation and who do not have cancer with HRD.
Bevacizumab, an anti-angiogenesis inhibitor that is given by vein, is also approved by the FDA for maintenance therapy of ovarian/fallopian tube/peritoneal cancer. In 2020, the FDA approved the combination of bevacizumab with olaparib for maintenance therapy in the first-line setting. If treatment with bevacizumab and chemotherapy has stopped or slowed the cancer, olaparib plus bevacizumab may be used as maintenance therapy for stage III or IV HGSC or endometrioid ovarian cancer in those with a BRCA mutation, have cancer with HRD (see above), or both.
If second-line platinum chemotherapy has stopped or slowed the cancer, maintenance therapy with olaparib, rucaparib, or niraparib (if determined the best option by your doctor) may be recommended in those who have not already received a PARP inhibitor. Although people with a BRCA mutation will have the highest benefit, others can potentially receive and benefit from a PARP inhibitor. Recent data show an overall survival benefit with olaparib, and data for the others is still pending at this time.
PARP inhibitors are taken by mouth daily. Common side effects are nausea, fatigue, vomiting, low blood counts, and altered taste.
-
Nausea can be treated with an anti-nausea medication. If nausea continues or worsens, ASCO recommends lowering the dose of the PARP inhibitor. This nausea usually lessens after 1 to 2 months of treatment.
-
A low red blood cell count, called anemia, should be monitored and may be treated with a blood transfusion. If the anemia still persists or gets worse, the doctor may lower the dose of the PARP inhibitor.
-
Similarly, white blood cell count will be monitored. If a low white blood cell count, called neutropenia, is severe enough and causes a fever or lasts at least 5 to 7 days, PARP inhibitor treatment should stop until the neutropenia gets better. In such cases, the doctor will lower the dose.
-
A low platelet count, called thrombocytopenia, may occur in those treated with niraparib. Lowering the dose of the PARP inhibitor or stopping treatment may be needed when this is ongoing or severe. If you have a low body weight or platelet count before starting niraparib, your doctor may recommend starting at a lower dose of niraparib to allow for better tolerance.
-
If lowered red or white blood cell counts continue even after PARP treatment is stopped, the patient should be checked for myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML). These rare conditions may be related to PARP inhibitor treatment or other cancer treatments.
This information is based on ASCO recommendations for “PARP Inhibitors in the Management of Ovarian Cancer.” Please note that this link takes you to another ASCO website.
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells.
Pembrolizumab (Keytruda) and dostarlimab (Jemperli) are a type of immunotherapy called immune checkpoint inhibitors. They work by stopping the ability of cancer cells to stop the immune system from activating, which helps the immune system destroy cancer cells.
Pembrolizumab is approved by the FDA to treat metastatic ovarian/fallopian tube/peritoneal cancers or cancers that cannot be removed with surgery and have high microsatellite instability (MSI-H) or DNA mismatch repair deficiency (dMMR). Tumors that have MSI-H or dMMR have difficulty repairing damage to their DNA, which can cause them to develop large numbers of mutations in their DNA. These mutations then produce abnormal proteins on the tumor cells that make it easier for immune cells to find and attack the tumor. These mutations are very rare in high-grade serous cancers (HGSC) and uncommon in other subtypes of ovarian/fallopian tube/peritoneal cancers. Dostarlimab is approved by the FDA to treat recurrent or metastatic ovarian/fallopian tube/peritoneal cancers that have dMMR and have progressed during or after previous treatment.
Talk with your doctor about possible side effects of the immunotherapy recommended for you. Learn more about the basics of immunotherapy.
Return to top
Hormone therapy
Rarely, hormone therapy, also called endocrine therapy, may be used as maintenance therapy for some low-grade serous tumors if they come back, or recur. These include tamoxifen (Soltamox) and aromatase inhibitors, such as letrozole (Femara), anastrozole (Arimidex), and exemestane (Aromasin). Hormone therapy is also used to treat stromal tumors, such as recurrent granulosa cell tumors. Learn more about the basics of hormone therapy.
Return to top
Radiation therapy
Radiation therapy is rarely used in general and not used as a first treatment for ovarian/fallopian tube cancer. It may be used to treat some people with stage I or II clear cell ovarian cancer after chemotherapy. Occasionally, it can be an option for treating small, localized recurrent cancer. It may also be an option for ovarian/fallopian tube cancer that has spread to other parts of the body. (See “Remission and the chance of recurrence” below for more information about treatment options for recurrent ovarian/fallopian tube cancer.)
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. The most common type of radiation treatment is called external-beam radiation therapy. This type of radiation is given from a machine outside the body. When radiation treatment is given using implants, it is called internal radiation therapy or brachytherapy. Proton therapy, which uses protons rather than x-rays to treat cancer, may also be used as an alternative to traditional radiation therapy. At high energy, protons can destroy cancer cells.
A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
Side effects from radiation therapy may include fatigue, mild skin reactions, upset stomach, and loose bowel movements. Most side effects go away soon after treatment is finished. Learn more about the basics of radiation therapy.
For more information on radiation therapy for gynecologic cancers, see the American Society for Therapeutic Radiology and Oncology's pamphlet (PDF), Radiation Therapy for Gynecologic Cancers. Please note that this link takes you to a separate, independent website.
Return to top
How epithelial ovarian/fallopian tube cancer is treated
As discussed in the Introduction, most cases of ovarian/fallopian tube cancer are epithelial carcinoma. Of those, a great majority are HGSC. In general, treatment for early stage, HGSC ovarian/fallopian tube cancer often involves surgery and adjuvant chemotherapy. Treatment for more advanced HGSC includes surgery with adjuvant chemotherapy and/or targeted therapy, neoadjuvant chemotherapy followed by surgery, or chemotherapy alone if surgery is not possible. Your doctor will recommend a personalized treatment plan for you.
Return to top
How ovarian germ cell tumors are treated
In general, the first treatment for ovarian germ cell tumors is usually surgery. In almost all cases, doctors can perform the surgery in a way that preserves fertility. Doctors may recommend adjuvant chemotherapy after surgery, depending on the stage and subtype of germ cell cancer. Chemotherapy usually consists of a combination of bleomycin (available as a generic drug), cisplatin (available as a generic drug), and etoposide (available as a generic drug) given by IV. The overall approach and medications given are similar to those used in male germ cell cancer, which is a type of testicular cancer. To learn more about this type of cancer, visit the Cancer.Net guides to testicular cancer and childhood germ cell tumors.
Return to top
How stromal tumors are treated
Stromal tumors are a rare form of ovarian cancer. They are found in the connective tissue that holds the ovaries together. In general, for a stage I stromal tumor, treatment usually consists of surgery only. For high-risk, early-stage tumors or stage III or IV disease, doctors often consider combination chemotherapy. Your doctor will recommend a treatment plan for you. You should discuss the potential risks and potential benefits of treatment options with your doctor.
Chemotherapy for a stromal tumor usually involves the combination of bleomycin, cisplatin, and etoposide, or carboplatin and paclitaxel. Chemotherapy can be used after surgery or for tumors that have come back after treatment, called recurrent disease. Researchers are looking at chemotherapy with carboplatin (available as a generic drug) and paclitaxel as alternatives. For recurrent disease, doctors may use hormonal therapy. Studies are being done to test tumors to find other, targeted drugs to treat ovarian stromal tumors.
Return to top
How metastatic ovarian, fallopian tube, and peritoneal cancer is treated
If cancer spreads to another part in the body from where it started, doctors call it metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
New treatments for these types of cancer include experimental combinations of chemotherapy, targeted therapy, and another type of systemic therapy called immunotherapy, also called biologic therapy. These combinations are designed to boost the body’s natural defenses to fight the cancer (see Latest Research). Because the benefits of these options are still being studied, their risks must be weighed against possible improvements in symptom relief and extending lifespan. Palliative and supportive care will be important to help relieve symptoms and side effects.
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. It is important to talk with your doctor about the possibility of the cancer returning. This is particularly important after treatment for ovarian/fallopian tube cancer, as many people experience recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence).
If a recurrence happens, a new cycle of testing will begin to discover as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, chemotherapy, and targeted therapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent ovarian/fallopian tube cancer.
How recurrent ovarian, fallopian tube, and peritoneal cancer is treated (updated 09/2022)
In general, chemotherapy is typically used to treat a recurrence of ovarian, fallopian tube, and peritoneal cancer. A primary goal of the treatment of recurrent disease is to reduce or prevent symptoms of the disease while keeping the side effects of treatment to a minimum. Treatment for people with recurrent disease is generally based on the time since their last treatment using a platinum chemotherapy drug. Platinum chemotherapy drugs include carboplatin and cisplatin. There is also evidence that surgery may be an effective option for certain patients with recurrent disease, and this should be discussed with your gynecologic oncologist. ASCO does not recommend the use of PARP inhibitors for people with recurrent ovarian cancer as an upfront treatment.
If the cancer comes back more than 6 months after platinum chemotherapy, doctors call it "platinum-sensitive disease." If the cancer returns in less than 6 months after platinum chemotherapy, doctors call it “platinum-resistant disease." Cancer that progresses during platinum chemotherapy is called "platinum-refractory disease." However, doctors are now starting to consider other factors than just the cancer's previous response to platinum chemotherapy when deciding which treatment to use for recurrent ovarian, fallopian tube, and peritoneal cancers. Talk with your doctor about their personalized treatment recommendations for you.
Treatment for platinum-sensitive recurrent disease
If the cancer is localized, additional surgery may be beneficial. Talk about this with your doctor. Surgery is usually considered only if the time following chemotherapy has been 1 year or longer. If the cancer comes back to more than 1 place in the body, chemotherapy is the appropriate next step. For people with platinum-sensitive disease (greater than 6 months from the last dose of platinum), clinical trials suggest using IV carboplatin and combining it with liposomal doxorubicin (Doxil), paclitaxel, or gemcitabine (Gemzar) may be beneficial.
Clinical trials showed the addition of bevacizumab to carboplatin combinations extended the time before the disease came back but did not change how long patients lived. You can discuss the risks and possible benefits of this approach with your doctor.
Treatment for platinum-resistant recurrent disease
In general, if the cancer returns in less than 6 months after platinum chemotherapy, the next chemotherapy is chosen from a list of medications that have all shown a similar ability to shrink the cancer. Doctors choose them based on possible side effects and preference based on the schedule of dosing. These medications may include, but are not limited to:
For platinum-resistant cancer, most doctors recommend single and sequential use (1 drug after another) of these medications, but they are sometimes used in combination.
Bevacizumab can be combined with liposomal doxorubicin, paclitaxel, or topotecan to treat platinum-resistant cancer. Doctors believe this is best used for patients who have received 1 or 2 treatments of chemotherapy and who do not have evidence of a bowel obstruction, as verified by a CT scan. By adding bevacizumab to the chemotherapy, the time before the disease recurs may be lengthened. You should discuss the risks and possible benefits of this approach with your doctor. Your doctor may suggest clinical trials that are studying new ways to treat your type of recurrent cancer.
Symptoms of recurrent ovarian, fallopian tube, and peritoneal cancer
The symptoms of recurrent ovarian/fallopian tube cancer are similar to those experienced when the disease was first diagnosed. The 4 most common symptoms are bloating, pelvic or abdominal pain, difficulty eating or feeling full quickly, and urinary symptoms (urgency or frequency). However, other symptoms may include persistent indigestion, gas, nausea, diarrhea, or constipation; unexplained weight loss or gain, especially in the abdominal area; abnormal bleeding from the vagina; pain during sexual intercourse; fatigue; and lower back pain.
In addition to monitoring symptoms, doctors may be able to diagnose a recurrence by measuring the level of CA-125 in the blood in people whose levels were elevated prior to treatment (see Diagnosis). CA-125 is a substance called a tumor marker that is found in higher levels in people with ovarian/fallopian tube cancer. In 95% of patients who have a recurrence, there is a rise in the CA-125 level. However, sometimes a recurrence can happen without an elevation of this marker, depending on the tumor type.
Whichever treatment plan you choose, palliative and supportive care will be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Return to top
Physical, emotional, social, and financial effects of cancer
Gynecologic cancer and its treatment cause physical symptoms and side effects as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer. Palliative/supportive care is different from hospice care, which is designed to provide the best possible quality of life for people who are near the end of life.
Palliative and supportive care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative and supportive care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative and supportive treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments, such as chemotherapy, surgery, or radiation therapy, to improve symptoms.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative and supportive care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
Cancer care is often expensive, and navigating health insurance can be difficult. Ask your doctor or another member of your health care team about talking with a financial navigator or counselor who may be able to help with your financial concerns.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Return to top
If treatment does not work
Recovery from ovarian/fallopian tube cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
Planning for your future care and putting your wishes in writing is important, especially at this stage of disease. Then, your health care team and loved ones will know what you want, even if you are unable to make these decisions. Learn more about putting your health care wishes in writing.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with your doctor or a member of your palliative care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Return to top
The next section in this guide is About Clinical Trials. It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.